17 | AWARE 4 – Agenda & Resources
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date May 20, 2022
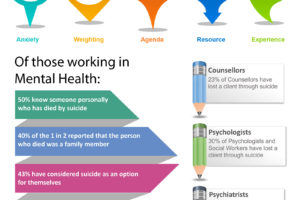
Transcript
Host: Good day, this is Mahi, your host, we are on to episode 17, Manaan provided an overview of the ASSESS module in Episode 13 and we explored attitudes to suicide. Episode 14 introduced the AWARE framework, and we discussed the impact of anxiety on decision making. We explored how attempts to provide hope and convey that “things will get better” might get in the way of thorough exploration in an assessment. Anxiety in assessors also manifests as reassurance seeking in the form of blanket safety questions – can you keep yourself safe, given the dynamic nature of risk they are often pointless and do little to actually address or mitigate outstanding risk. In episode 15 we discussed two mental spaces, rational and rationalizing. Rational is information first, decision later and rationalizing is decision first followed by selection of information to support the decision or action. This theme plays out in all the AWARE factors. We then had our third Guest Episode – Shazzy Tharby, a fairly long content heavy episode in which Shazzy outlines some of the challenges of supporting Autistic people in suicidal crisis and how those challenges may be overcome. In Episode 16 we returned back to the PROTECT course content and we explored how much weighting assessors put on certain diagnostic groups namely personality disorder, and substance misuse and how suicidality in these groups often count for less, also how an acute course of illness gets more priority than chronic although those who are chronically unwell may have lost touch with hope and finally how suicidality caused by modifiable social factors are often considered by healthcare staff as outside their core remit of work and these patients end up receiving less support than those with a clear cut biological mental illness. Manaan, what did I miss?
Expert: Not much, that’s an excellent summary, in the last episode we also outlined different care approaches so the response to acute suicidality should be like a response to a person having a Myocardial Infarction, jump in and do whatever needs doing, the response to chronic suicidality is more along the lines of supporting someone with severe diabetes, helping the person to take control and supporting them through appropriate education and safety planning that suicidal urges can be mastered and finally the most risky, acute on chronic presentations which is like a severe diabetic person having a heart attack, in these patients it is really important to predefine what an escalation of risk looks like. Also remember that all three subthemes described like a diagnosis of borderline personality along with substance use, a chronic course and a host of social issues may be present in the same individual, and for each of those factors if the risk is minimized we may be overlooking the needs and risk in a person who may be perilously close to an attempt.
Agenda
Host: This is a nice segue way into the next AWARE factor – Agenda, cause often patients with personality disorder and substance misuse are considered to have an agenda, like are they trying to get admitted or they are trying to que jump and get a back door detox, sometimes these agendas are related to social factors like they have got housing issues and are just attempting to get rehoused through an admission and so on. Were these the kind of scenarios that were highlighted under the agenda theme of the AWARE study?
Expert: Yes that is correct. Essentially we want assessors to pause and think HOW OFTEN ARE YOU RESPONDING TO AN AGENDA IN AN ASSESSMENT AND IS IT SKEWING THE OUTCOME?
Host: How would you define an agenda?
Expert: Put simply an agenda is a desire or motivation to achieve a particular outcome. Sometimes they are clearly stated and other times its implied or perceived by the assessor. What we found in the AWARE study was that once you pick up an agenda it begins to influence information processing.
Host: So that relates to your opening statement about agendas when you asked our listeners to pause and think, how often are you responding to agendas?
Expert: Yes, it does, throughout the assessment the assessor is interacting with people, processing and accepting the referral, triaging, collating information, and the face to face assessment itself with the person in distress and their family. During these activities’ agendas may be picked up in a referrer / patient/ carer by assessing practitioners, to which they end up consciously or unconsciously responding.
Host: How does an assessor know that they are responding to an agenda?
Expert: It is not unusual for an assessor to try and work out, what are the person’s need? Why do they want this? Why now? Now that is fine, that’s what an assessment is, assess to establish the needs, and you can change the person to the referrer, patient, family member etc. but when you begin to wonder is there a secondary gain, is there a hidden agenda, essentially when you begin to second guess what someone is saying as the reason for their referral, you can rest assured that you feel there is an agenda.
Host: You mentioned agenda in the referrer, what agenda could a referrer have when requesting an assessment other than getting the person assessed?
Expert: Rightly or wrongly, assessors very frequently felt that the referrer had an agenda. Generally they were judgement calls on Referral Appropriateness. Referrer credibility was often scrutinized when reviewing a referral, this varied from conclusions about a referrer’s risk taking to passing the buck as they were going on leave and wanted someone else to take responsibility.
Host: What kind of statements did you get in the AWARE study?
Expert: So we had statements like: “…I felt that the reasons for the referral weren’t really appropriate. He was someone that they’d (Locality Team) only seen twice, the reason for referral was that he was being actively suicidal. But I felt the risk was kind of raised so we’d go and see him…” Often we would pick up an implied statement – You are passing the buck to me without doing your part
Host: What kind of statements did you get that related to patients having an agenda?
Expert: I have a nice example here: “…Suicidal ideation was in the context of depression… because she has a child, so I think it’s always worth having a look when there’s a child, I got the clear sense that she was downplaying it as she did not want social services involved, we needed to do something…” So in this example the assessor felt that the patient was not being very open as she was worried about her child and social services involvement.
Host: So in the first statement the assessor’s interpretation of an agenda resulted in decreased sensitivity to suicide risk i.e. they have only seen her twice and have not done their part and in the second she might be trying to conceal her symptoms increases the assessors awareness of risk related factors.
Expert: Yes, almost diametrically opposite impact. Altered care responses were most obvious when judgement calls were made about the appropriateness of the referral. Assessors often did not accept the referral if they felt that the referrer had not done their part, and even if they did, it impacted on the assessment outcome. The risk and the need in the person in distress does not change with whether there is any truth to the claim of lack of diligence on part of the referrer.
Host: And then there was the opposite where they might have got over involved or more intrusive or more risk averse if they felt that the patient did not want to engage for some reason.
Expert: True, attempts to avoid hospitalisation were picked up and responded to fairly robustly. Other than influencing risk sensitivity there was also a spectrum in terms of the type of response, sometimes the response was positive, and other times negative, which actually escalated the risk.
Host: Can you provide an example of a perceived agenda in a patient which actually increased the risk.
Expert: These were primarily the implied requests, e.g. for admission in people with a diagnosis of borderline personality disorder were often met with skepticism.
Host: Given inpatient beds are such a scarce resource and in the previous episode you talked about how the focus for chronic risk, as in people with borderline personality should be psychoeducation and safety planning, rather than admission at every presentation, isn’t skepticism warranted.
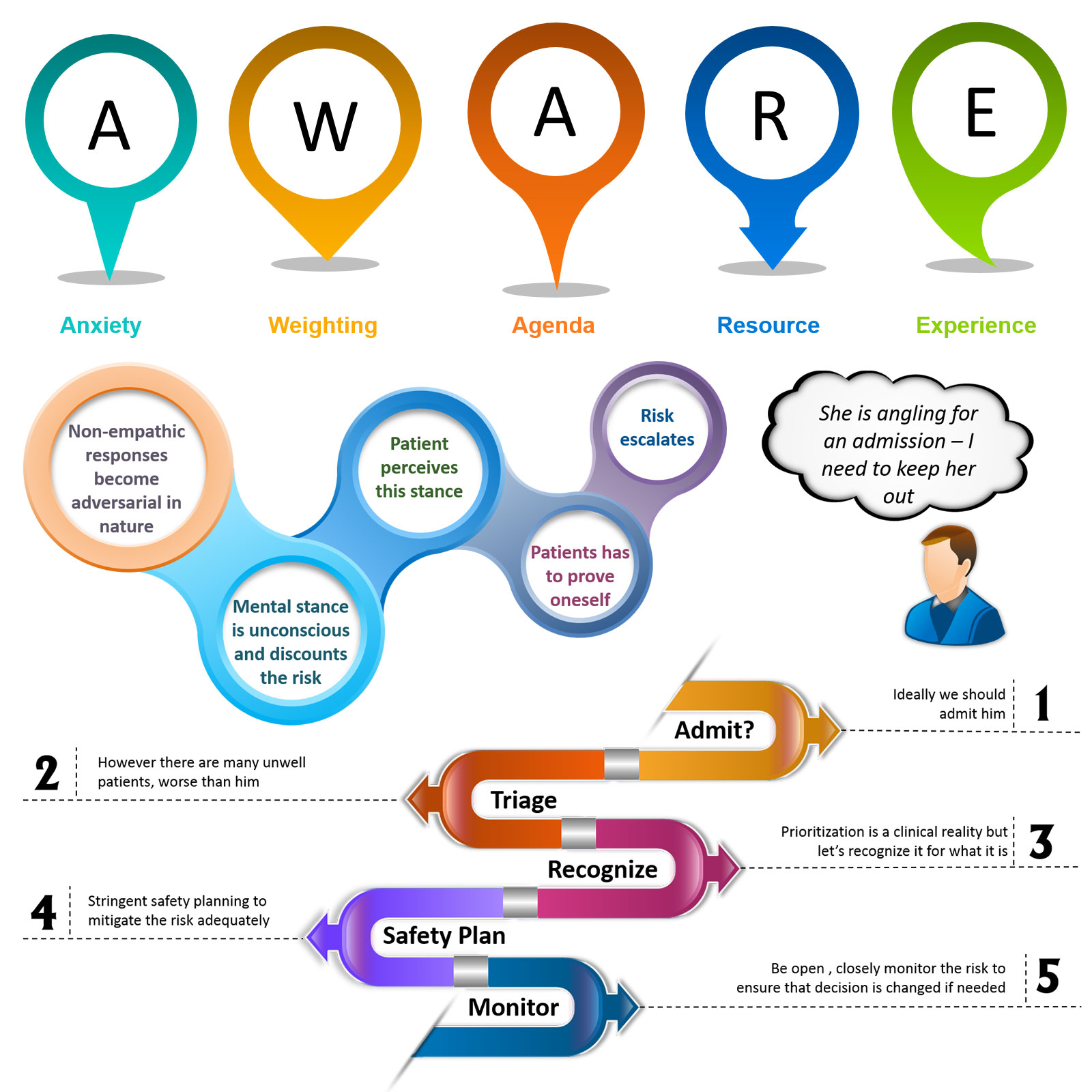
Expert: Yes, it is but it is the way in which the conversations pan out. When we have finished all the aware factors we will do some case based discussions regarding what and how to communicate with a person in crisis who has a borderline personality disorder. In brief certain agendas brought about a non empathic response, for example ‘she is angling for an admission, I need to keep her out of hospital’. This became adversarial in nature, and the study revealed that the assessors were often unconscious of this mental stance. But the patient perceived this stance very quickly, remember people with borderline personality are hyperaware of abandonment and rejection. So when they perceive this stance in a clinician who is discounting how unsafe they are currently feeling, they feel a pressure to prove their suicidal distress, and this escalates the risk in the situation.
Host: What about positive responses?
Expert: Our study revealed that carer requests regarding their ability to care, or struggling with burnout particularly when openly stated received a positive and empathic response from assessors. This was of course perceived as positive and helped with relational safety and carer confidence. Here is a statement relating to a spouse: “I think her husband felt that she needed to come into hospital …he was quite distressed by what she had done again. He felt it was a heavy load to carry at the moment. Too much to cope with…” One can see the thinking of the assessor that the carer is desperate for a break and needs our help, perhaps to keep caring for the longer run.
Host: So openness brought out a positive response.
Expert: This is true in all walks of life. Yes, generally if the referrer, patient or carer were open about what they wanted assessors seemed to pay heed to the request and tried to accommodate it, its when they felt that someone was trying to work the system that their position would harden and the perceived agenda would begin to influence the information processing and the decision that was arrived at.
Host: So perception of an agenda leads to a particular kind of response that may escalate the risk.
Expert: Yes we do want assessors to reflect on whether their response to the person they are assessing whether that is escalating the risk in anyway. The AWARE study clearly showed that assessor responses had a range of foreseeable as well as unforeseeable outcomes. From making a patient with borderline personality disorder feel that now they had to prove their distress by self harming to a patient downplaying their symptoms in response to a conservative approach in an assessor. We also saw the converse in terms of empathic responses to stated or perceived agendas, such responses were clearly perceived as helpful by the person, the family, and the referrer.
Host: So let’s pull this together in terms of what assessors need to do.
RECOMMENDATION
Expert: Assessors need to mindfully scan themselves ‘am I picking up an agenda’. If they find one, avoid the temptation to rationalise their response like this is just an anxious GP who refers everyone or this case manager is going on leave so is referring everyone on their caseload. Such judgement calls change the outcome of the assessment without addressing the actual cause for the presentation, i.e. the risk has remained the same or might be even worse as now the patient feels that the hope they had for help has now been dissipated. This is not an uncommon theme in serious incident reviews where a patient attempts to take their life after a presentation for admission or what they believed would result in an admission. So if you perceive an agenda, make the implicit – explicit, seek clarity from the patient and their family, bring it out into the open as to what you feel may be there expectations. Do it with sensitivity and have an open and honest discussion with them regarding the reasons for why they might feel the way they do. This is a fairly nuanced discussion and we will discuss this further when we do a case based discussion.
Resources
Host: This moves us on to the penultimate theme, resources.
Expert: All AWARE factors are interlinked, resources impact agendas and agendas and responses to agendas often relate to resources. So the next question we want to ask our listeners is DO RESOURCES IMPACT YOUR DECISIONS?
Host: In healthcare systems with finite resources this must have a considerable influence on care decisions that are made.
Expert: Actually our research revealed that most practitioners were quite conscious about the impact of resources on decision making. So that is good. But most took the stance that they tried their level best to carry out the assessment independently of the bed state. When directly asked about bed pressures influencing decisions most practitioners said no it didn’t. Given the crisis team gate keeps beds in the UK, we asked clinicians why then did they feel the need to go and check the bed state before going out for an assessment.
Host: So what kind of responses did you get?
Expert: All sorts, from it’s a long standing habit to get a sense of the overall system, how might my day look like. Practitioners indicated that if a patient was very unwell they would ensure that they get a bed, by that they meant that if it was necessary to create a bed by facilitating an early discharge they would do so.
Host: So they were saying that decision to admit was not resource led but a discharge could be brought forward because of lack of beds in the system.
Expert: Yes they were saying that but we clearly saw fluctuations in the threshold for admission based on bed availability.
Host: What kind of statements did you get in the AWARE study?
Expert: Here is one: “We knew there was a bed, actually we knew there were plenty of beds on the ward, so we kind of thought, you know what this lady could just do with a break and some more assessment of her depression” So the implied bit of the statement is that we admitted her for a break because there were beds, if there weren’t any most probably we would not have admitted them.
Host: That is for something concrete like for beds how about home treatment?
Expert: We actually saw the same phenomenon for home treatment, when the team was extremely busy the threshold to be taken on significantly went up compared to the time when the team had fewer patients in home treatment. In fact in the study a couple of clinicians got offended when asked about the impact of workload on the decision to be taken on or not for home treatment.
Host: Do you have an example?
Expert: Here is one in which the clinician said : “It had no bearing on the decision (not to take a suicidal patient on for home treatment). What does that mean if we were short staffed we wouldn’t have taken him? No it had no bearing on it whatsoever.”
Host: So how should assessors tackle this tricky issue of resources?
Expert: Stay Rational and Stop Rationalising
Host: That was a bit cryptic, can you elaborate.
Expert: Look, it is not uncommon a situation where four patients might be competing for a single bed. Clinical triage and prioritisation is a reality of modern day practice. However rationalising or dressing up a resource led decision as one that has been made in the best interests of a person in distress actually does little to enhance safety, if anything it makes the situation worse as it covers up for a potentially dangerous situation.
Host: So do not rationalize away your decision to say not admit as the best outcome for the patient.
Expert: We hear rationalizing statements all the time, when there are no beds we might say we should try to use the least restrictive option and treat at home which is the least restrictive option, this is in keeping with recovery principles. In home treatment we might say it is time to discharge as staying too long with us will create dependence and our team only provides short term support, when the reality is we are trying to manage the high work load of the team. In a community team with a long waiting list for psychological treatments we might say previously for this person therapy has had very little impact they might be better served with practical support from the third sector. And so on, these rationalizing statements make us feel better about the decision but do very little to actually address the cause with which the person is presenting or the risk that they pose to themselves. So stop rationalisng.
Host: And instead stay rational?
Expert: Yes stay in the rational space, you might make the same decision but the way in which you arrive at the decision is quite different. For example the assessor might think Ideally we should admit him, however there are many unwell patients, worse than him, so the assessor understands that prioritization is a clinical reality but they also recognize their decision for what it is. So they engage in stringent safety planning to mitigate the risk adequately. They stay open to the idea of a future admission and closely monitor the risk to ensure that the decision is revisited or changed if needed.
Host: What you are saying is stopping onself from rationalising would make practitioners engage in a much more stringent safety plan one in which they actively look to mitigate the impact of a resource led decision like not to admit someone due to bed unavailability.
Expert: Absolutely, BEWARE OF THE TALES WE TELL OURSELVES TO MANAGE OUR COGNITIVE DISSONANCE, think for a moment HOW WOULD YOUR THOUGHTS AND ACTIONS LOOK LIKE, IF YOU COULD BE OPEN ABOUT THE CLINICAL REALITIES IN WHICH WE WORK? Now most organisations do not have the maturity to call a spade a spade. But if we are to make things better and safer for the person in suicidal distress we will make the implicit explicit, we will accept we make resource led decisions frequently, we will not rationalise it away, in fact we will have an open and transparent discussion with the patient and family that ideally I would have like to have admitted him, but we haven’t got a bed so lets all work together to make it as safe as possible and we can revisit the decision in future and keep in under close monitoring. We will then document it for what it is and take steps to reverse the decision as soon as the constraints on resources has decreased or if things deteriorate further.
Host: The kind of things you are talking about, is the stuff of nightmares for a hospital administrators.
Expert: Yes I know, everyone gets worried about legal consequences and law suits if a life is lot or there is a bad outcome and there is a documented resource constraint in the patient records, but these resources constraints are impacting clinical decisions every day. If anyone thinks that is not the case, they are lying to themselves and are actually standing in the way of patient safety in the short term and in the long term the hard yards that are needed to address these resource shortages.
Host: I think we have run out of time today. We have covered two very important AWARE factors, agenda and resources. Remember the show notes and images will be at the blog on www.progress.guide and you can get the PROTECT suicide prevention Guidebook from Amazon. There are number of online video courses as well. Pause and think when you perceive an agenda in a person, does it change the way in which you respond to them. Think about routine normal life first and then take that awareness into the clinical setting. Are you more likely to keep a request if you feel that someone is being open and honest with you. Also spent time reflecting on the last week, last month, maybe even last year. What kind of rationalising statements you might have used when faced with resource constraints. Pretty certain everyone does struggle at times with workload and does that impact the threshold for entry into your service. Share your musings with us. Tweet your thoughts about agenda and resources and tag #GuideProgress. It helps get the word out about the podcast to more professionals and support progress to practice. You can email your thoughts to us at admin@progress.guide with your suggestions and comments particularly if you have questions and want us to cover certain topics in the discussion. In the next episode, we will cover experience the final factor in the AWARE framework. We will also cover creep-crash-crawl, a common phenomenon but covered in a unique fashion within PROTECT. Please spread the word, you can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Helping healthcare professionals become aware of their decision making processes is an essential step in creating a workforce that is self-aware. Remember together we can make a difference. Tune in next Friday and we will discuss how your past experience shapes your clinical decisions. Thank you for joining us today and keep spreading the word.
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience