16 | AWARE 3 – Weighting
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date May 13, 2022
Transcript
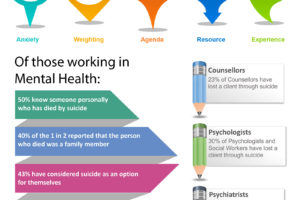
Host: Good day, this is Mahi, your host, we are on to episode 16, we began the ASSESS module in Episode 13, Manaan provided an overview and we started looking at attitudes to suicide and why awareness regarding where one stands is so important in terms of care delivery. In Episode 14 we went deeper into the first chapter of ASSESS, appraise decisions and began the AWARE framework. We discussed the impact of anxiety on decision making and how assessments have a dual role, the overt stated one i.e. to assess and the subtle implied one i.e. to contain the crisis and how these two functions can be at cross purposes and how anxiety of unearthing things that are difficult to contain may get in the way of a full through exploration. In episode 15 we built on this concept further and discussed two mental spaces, rational and rationalizing. So rational is information first, decision later and rationalizing is decision first followed by selection of information to support the decision or action. Manaan you believe this is the key insight from the AWARE study.
Expert: Absolutely, awareness of these two mental operating spaces is critical in gaining a greater understanding of what influences clinical decisions. They play out through all 5 aware factors. By the end of the AWARE framework listeners will realize that rational vs rationalizing is the glue that holds the five factors together.
Host: I love the diagram in the PROTECT book of those faceless people, the rational professional looks at all the jig saw pieces and makes their decision and the rationalizing clinician makes their decision and then points out specific pieces from the jig saw puzzle that supports their decision, while neglecting the rest.
Expert: Yes, my colleague and co-author of the AWARE paper absolutely loves that image, she was the one who did most of the thematic analysis of the assessor interviews and she says that the image captures what she was noticing in the answers given by professionals, post assessment as to why they decided to send someone home or why they admitted someone. They had made the decision quite early in the process and then zeroed in on information that supported their decision.
Host: If you don’t know where to access the images they are available at the podcast blog at www.progress.guide , you will also find the show notes, the key messages and the messages in images. Also you can get the PROTECT Guidebook from Amazon to read along. I keep reinforcing that the images are particularly helpful for visual learners and help with retention. We have worked hard to make the PROTECT training as intuitive as possible to aid with retention and images and acronyms are all part of that concept retention process that we pay a lot of attention to in the live or online training. Also do not forget to subscribe and rate us on spotify or apple podcast, share the episode on link din and twitter it helps us get the word out. And do send through questions, topics and guest interview suggestions to admin@progress.guid . Let’s get started with the crux of episode 16, the next aware factor, weighting.
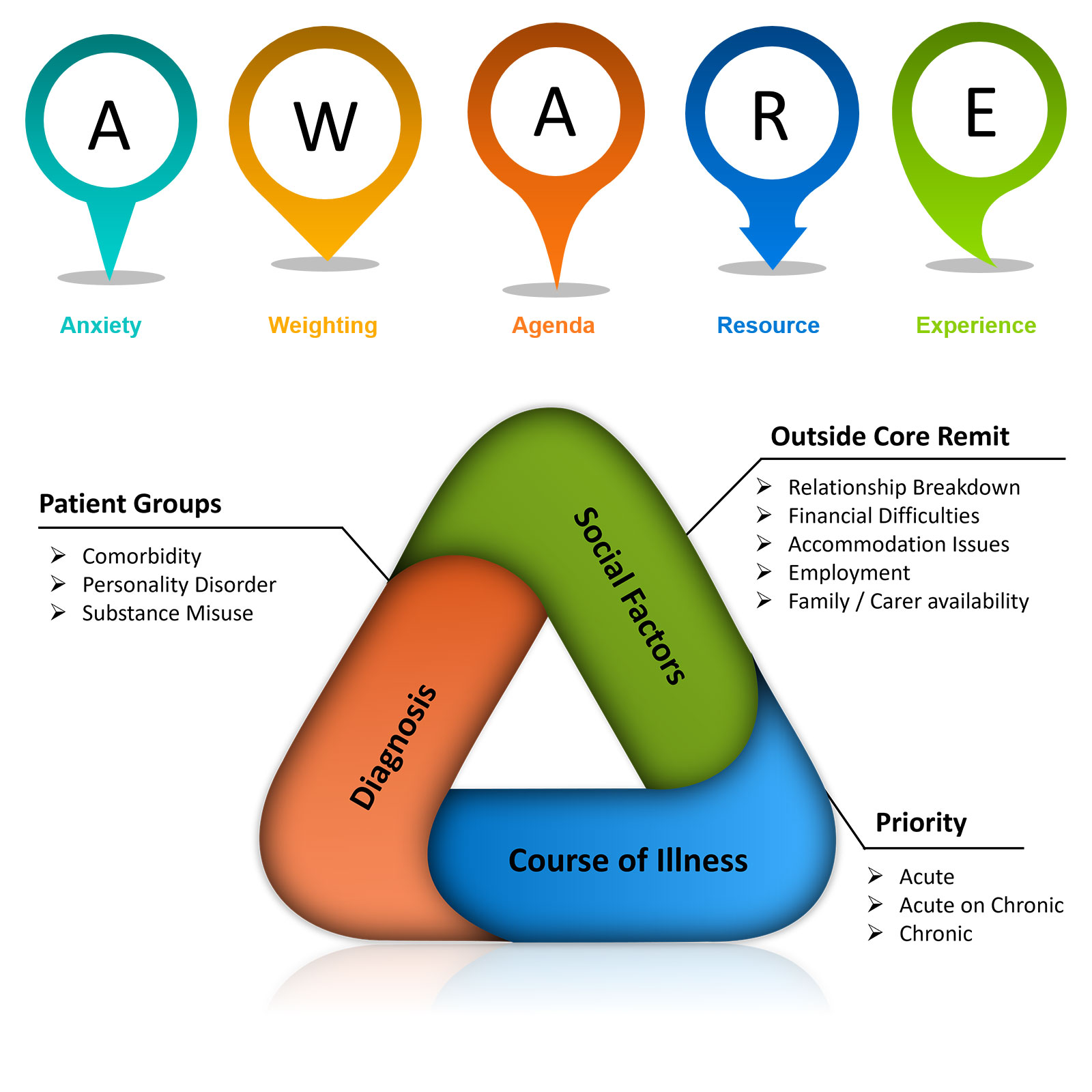
Expert: Yes, weighting is the second theme in AWARE. The presence or absence of certain factors made assessors view suicidal distress in different light. These factors were: diagnosis like suicidality in personality disorder and substance misuse counted for less, course of illness – acute presentations trumped chronic ones and social factors which were considered to be outside the core remit of mental health work.
DIAGNOSIS
Host: So, let’s begin with diagnosis, you were saying that suicidality in certain diagnosis counted for less.
Expert: Yes a rational observation of suicidality would have revealed, similar or even higher risk due to having a personality disorder and/or substance misuse, but we noticed that somehow risk was minimized in the assessment process and patients with these diagnosis were comparatively provided less intensive support options and were often referred back to their referrers for ongoing support or encouraged to reengage with their current community supports or referred on to other agencies outside secondary care.
Host: And the comparator here is those who were clinically depressed without personality disorder and/or substance misuse.
Expert: Yes, and also other conditions like depression in someone with schizophrenia or depression with someone with a bipolar condition. The thematic analysis revealed statements like “He’s a heavy cannabis user, which he uses to self-medicate with his anger difficulties. We gave him advice on alcohol making him impulsive, what else can we do.”
Host: This is in response to queries about why they might have not been admitted or taken on for home treatment.
Expert: Yes, and the degree of suicidality might have been very similar. In fact the risk is higher if you look at severe Personality Disorder, that has a standardized mortality ratio from suicide of 45.1, highest amidst all diagnostic groups. This is in comparison to 19.7 for depression, yet statements like “she has a borderline personality disorder and is on the waiting list for MBT in the community, that is going to be the mainstay of treatment, what is to be gained by a short stint in home treatment or an admission.” But the risks of life lost through suicide are actually higher because of personality disorder.
Host: What is MBT?
Expert: Sorry Mentalization Based Treatment, we had invested quite heavily in MBT training of staff in the Community Personality Disorder Pathway in Cambridge and that was one of the main therapeutic options on offer. In essence what they were saying was not incorrect, longer term therapy is the answer, but what about short term support, the question kept coming back, did the diagnosis influence the actual clinical decision not to take someone on for short term support.
Host: You also mentioned substance misuse, how does the standardized mortality rate for suicide in people who are using substances compare with depression.
Expert: It is different for each substance, for opioid use is at 13.5, it is lower than 19.7 of depression but 13.5 is comparable to that of lung cancer from smoking, but suicidality in people using substances often counted for less. This may relate to frequent presentations at A&E or even a separation in the UK between mental health care and addiction services. Over the last 15 years contracts for addiction services have gradually gone to the NGO sector and there is this artificial divide between mental health care and addictions support.
Host: And do patients often fall in between?
Expert: Yes absolutely, you end up having a system that where parts of the system go, not mine – yours and the other goes not mine – yours. So for those with dual diagnosis and most in need, instead of having a service that is step up, essentially you get a step back service, everyone says not mine. One of the joys of working in the NHS is how integrated care is across the primary – secondary divide, I cherish that every day now that I do not enjoy the same luxury in Australia where primary care and secondary care are not integrated but in the UK care for those with dual diagnosis has been fragmented by taking addiction services away from the NHS, not to mention the impact of that on the training of future addiction psychiatrists and nurses etc. Anyway I am digressing, as you can see I have very strong views on the split between mental health care and addictions and I feel that had a part to play in the weighting of symptomatology we noticed in the AWARE study in those with substance misuse problems and concurrent suicidality. In fact both for personality disorder and substance misuse the risk of death through misadventure, impulsivity and repeat attempts is far greater than in those with depression.
COURSE
Host: In the Weighting theme, after diagnosis the next sub-theme you mentioned was course.
Expert: Yes. We found that an acute presentation where there has been a step change trumped acute on chronic which trumped chronic presentations. The clinical reality is that people who have been chronically unwell, or have been unwell for a while start to loose touch with hope and could be at as much risk or at a higher risk than those who get acutely unwell. Acute risk seemed to get more priority.
Host: Was there a relationship between the diagnosis and course?
Expert: That is a legitimate question as often people with personality disorder and alcohol misuse or substance use have ongoing risk and present repeatedly or frequently in crisis. One can see why there might be a degree of desensitization to the risk with which they are presenting due to the chronicity on display. In short yes, when there is an acute escalation in risk the assessors felt the need to do something definitive but for chronic risk there was a sense of not much has changed, why now.
Host: What kind of statements did you get in the qualitative analysis?
Expert: For acute risk we had statements like “…she was presenting as quite labile… was quite unsettled, agitated, disinhibited,… we have to do something.” For chronic risk we had statements like “I didn’t think it was an appropriate referral, he has long term on-going problems, more could have been done by the locality team, before referring.” You can hear the two contrasting approaches in acute risk we need to do something now but in chronic risk it is someone else’s responsibility, why are they being referred to the most expensive bit of the system whose job is to deal with the most acutely unwell. But how do you say that the chronic risk has gone past a threshold that something definitive needs to happen.
Host: Essentially you are saying that there is a natural predisposition in crisis professionals to take more seriously acute presentations but that it is important to remember that people who have been chronically unwell may have completely lost touch with hope and might feel more trapped than those who are acutely unwell and that risk needs to be taken seriously.
Expert: In the actual PROTECT training, we run case study simulations on a model of suicidality called STEPS in which we take trainees through the different stages of predisposition, ideation, intention, action, contemplation in post action, repeat action and back into life in motion with a safe recovery. We will talk about this in detail in a future episode as to how, static, stable, dynamic and fluid factors interact, however one thing that always stands out for me is to how limited an understanding participants have of the different approaches that need to be taken for acute risk, chronic risk and acute on chronic risk.
Host: Can you tell us more about these different approaches.
Expert: It’s a bit difficult to explain without the STEPS diagram, I guess listeners can imagine a tiered system of progression. We will talk about this later on as well when we discuss progression of suicidality from ideation to intention to action, please remember that it is not sequential in real life and people fluctuate all the time between these tiers, but say for illustration purposes if you are dealing with acute risk, that involves someone going in a short period of time from life in motion or predisposition through to ideation, intention formation and action, so a sudden peak in risk, now our response to this needs to be like a response to someone having a myocardial infarction.
Host: So, taking definitive steps, like in a patient with chest pain having a heart attack.
Expert: Yes, so jump in and do what needs to be done. In chronic risk though like someone with personality disorder or chronic depression, there suicidality may be going along with minor fluctuations going in between ideation and intention sometime peaking into action. Now every time they present in crisis it will be inadvisable to admit them, the response to them however needs to be equally thorough but is qualitatively different to the one of a patient having a heart attack. I think of them as patients who have a severe diabetic illness and they need rigorous support to help them stay on top of their diabetes, a lot of that is self-monitoring and self-regulation, taking adequate insulin, eating appropriately, avoiding hypoglycemic states, getting adequate wound care if they get a cut and so on.
Host: So, for chronic risk, rigorous support like in severe diabetes, but care that is primarily led by the person and the person has to take charge of their recovery.
Expert: Yes, so we draw on the person’s internal coping strategies, help them understand, that suicidal urges come in waves, every time they can use an internal coping strategy successfully, they learn that these urges can be mastered, so the focus is very much on learning distress tolerance. There may be a temptation to rationalize the risk away as low or non-existent as not much has changed but people with chronic risk need rigorous safety planning, particularly as it is more likely that they would be managed in the community. So a lot of work, and maybe even more work needs to go into chronic risk management than acute risk management where you step in and take control.
Host: And this additional work is to prevent people with chronic risk tipping into suicidal action, assuming if you are in that ideation – intention tier of the STEPS model it will not take much to tip one over into a full blown crisis.
Expert: That is exactly correct, understanding triggers, early warning signs, when to use internal coping strategies, when to use external coping strategies, when has it become a crisis, when is it an emergency, so clarity over what to do when and with whom is essential. So, a lot of work involved in mitigating chronic risk, just like in supporting people with severe diabetes.
Host: So, for acute risk, deliver care like you would for someone having a heart attack and for chronic risk, deliver care for someone with severe diabetes, now what about presentations which are acute on chronic?
Expert: Put simply this is like caring for those with a severe diabetes in the midst of a heart attack. So they really should be the top of your response list but unfortunately if you are not able to differentiate acute on chronic risk from chronic risk one is bound to take the wrong approach. That is why it is so important to predefine in a person centered way for each individual what does acute on chronic look for them, so for someone who self harms it might be that their frequency of self harming goes up from once or twice a week to daily or they go from self-harming on the concealed parts of their body to on their neck and face or their cuts are getting quite deep and are no longer superficial. This discussion needs to be undertaken when the person is calm and almost like an advanced directive care should be preplanned for these situations. In my experience designing this safety net actually decreases the frequency of such crisis.
Host: I know that you talk about this kind of ultra high risk scenarios in the suicide prevention training for GPs and primary care professionals.
Expert: Yes, it’s a training program called LIFE, designed for primary care folk, they are the ones who deal with a lot of chronic ongoing risk and doing this work up when the going is good provides clear trigger points of when to escalate to secondary care for short term intensive crisis support for the difficult period to subside and for them to return back to primary care. Supporting people with Personality Disorder is a challenge even in secondary care, so you can imagine how difficult it is in primary care with 10 minute appointments, but remember it can be a sequence of 10 minute appointments, that is what management of chronic risk involves and if one or two of those 10 minute appointments are utilized for forward planning a lot of risk can be managed.
Host: This has been a really informative and an in-depth discussion on the course of illness, acute risk remember heart attack, chronic risk remember severe diabetes, acute on chronic risk, think heart attack in a person with severe diabetes.
Expert: And make sure that there is clarity on how you will spot the heart attack in a person with diabetes. I feel we have gone of at a tangent from the AWARE factors.
Host: But it was important to understand the different approaches or else people might just rationalize away chronic risk as low risk rather than do the safety planning work up that is needed. Have we covered the course of the illness discussion?
Expert: Yes, I think we have.
Host: That brings us to the third of the subthemes in weighting, social factors.
Social Factors
Expert: Yes, responding to suicidal crisis emanating from social factors like Relationship Breakdown, Financial Difficulties, Accommodation Issues, Employment difficulties, Family / Carer availability seemed to be quite low on the priority of the assessors. Suicidality in people with a clear cut biological illness (like depression, bipolar disorder) were taken more seriously than those who were overwhelmed by life circumstances which were generally social in nature.
Host: Why do you think that was?
Expert: This is speculative but in my honest opinion, my feeling was that the assessors did not consider responding to a social crisis as part of the remit for mental health care staff. There was a strong feeling that we are here to treat mental illnesses.
Host: Did that come out in the thematic analysis?
Expert: Yes, there were statements like “…social support impacted the decision making… no significant friends or family. She receives no support from care services with regard to her son… She is single, financially lacking and on benefits, lacking social support. She has physical illnesses with a lot of symptoms… but not for us really…” The degree of suicidality may be quite similar to someone with depression, but suicidality emanating from a social crisis seemed to count for less in terms of a mental health response, whether that be an admission or home treatment support. Generally onward referrals were made to non health or non-statutory sector, which in many cases were appropriate as the practitioners were trying to remedy the cause of the problem.
Host: To bring all of this together, what should professionals do to stay in the rational space and respond appropriately rather than rationalise away risk as low or not much has changed.
Expert: Well, we will keep coming back to awareness through reflection and reflective practice. One needs to be aware of prejudices they hold regarding certain diagnosis. Also, they need to remain mindful of chronically unwell people, losing touch with hope. Finally social factors are modifiable and addressing them proactively can help resolve the crisis effectively.
Host: So, pause and think:
- DO YOU TAKE SUICIDALITY LESS SERIOUSLY IN CERTAIN DIAGNOSTIC GROUPS?
- DO YOU TAKE SUICIDALITY LESS SERIOUSLY IF THERE IS NOT A STEP CHANGE IN PRESENTATION?
- DO YOU TAKE SUICIDALITY LESS SERIOUSLY IF THEY ARE OVERWHELMED BY SOCIAL PROBLEMS?
BECOME AWARE OF YOUR PREJUDICES
Expert: There is also the bit that we discussed about how acute on chronic risk trumps all other kinds of risk and the different approaches that one takes to acute, chronic and acute on chronic risk.
Host: Yes, I absolutely loved the metaphor of responding to a heart attack, building self management skills in someone with severe diabetes and then rapid detection and response to a heart attack in a person with severe diabetes.
Expert: That’s a wonderful summary, all three subthemes, a diagnosis of personality disorder and/or substance misuse, chronic course and a range of social challenges may exist in the same individual. Now each one of these factors that actually increase risk and the risk may not be just additive it may be multiplicative. But in your mind somehow due to their diagnosis, chronic course and social causation you are just seeing more reasons for why a mental health response is not warranted, you can see how someone who is perilously close to taking their life may be left unsupported.
Host: That is an even better summary and a sobering thought to end episode 16 on. Today we have looked at Weighting, the second AWARE factor and the different approaches to acute, chronic and acute on chronic risk. Pause and think, how might this knowledge bring progress to your practice. When was the last time you assessed someone in whom these factors might have been at play. Did these factors influence your decision in any way. Did you stay in the rational space and notice all the factors, the overall escalating risk in the individual, and then make a judgement call or just noticed each factor on its own, and used it to justify why a crisis response was not warranted. Watch out for them at the next assessment. How do you respond to those with a personality disorder or those who have presented 3 times that week intoxicated to the emergency department? Do you find yourself saying in your thoughts, oh well not much has changed since the last presentation, pause and think, are you talking about chronic risk and they keep representing because no one has actually done the necessary safety planning work needed to manage chronic risk. What about social factors? Do you consider these modifiable factors as part of your core remit or not? The social determinants of health are such an important pillar of suicide prevention work, what should be your contribution. Share your musings with us. Tweet your thoughts about weighting and tag #GuideProgress. It helps get the word out about the podcast to more professionals and support progress to practice. You can email your thoughts to us at admin@progress.guide with your suggestions and comments particularly if you have questions and want us to cover certain topics in the discussion. In the next episode, we will go through the remaining factors in the AWARE framework. You can access all the information at www.progress.guide. You can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Helping healthcare professionals become aware of their decision making processes is an essential step in creating a workforce that is self-aware. Remember together we can make a difference. Tune in next Friday and we will explore how perceived agendas impact clinical decision making and depending on time the rest of the AWARE framework. Thank you for joining us today and keep spreading the word.
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience