18 | AWARE 5 – Experience
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date June 3, 2022
Transcript
Host: Good day, this is Mahi, your host, we are on to episode 18, we hope you enjoyed the guest episode with Dr Miguel de Sexias. His account of his journey from Cambridge to Saigon was fascinating.
Expert: Yes it was, apologies for the poor sound quality at certain parts of the interview, we tried to correct the drop outs as much as possible but the content was soul stirring. Miguel used this metaphor of proactively putting one’s foot through the door as a way of creating enough friction between suicidal thoughts and the person’s reasons for living. And later on went on to elaborate that the foot through the door shouldn’t be like a pestering salesman but one where permission is sought in a collaborative fashion. To me that captured all the things we say about relational safety.
Host: I also found the conversation about expats who were trapped amidst freedom quite a fitting oxymoron.
Expert: Yes they could move about within Vietnam with freedom but could not leave the country, so this idea that if something happened they could just return to their homes in the west at a moment’s notice was taken away. Maybe this is something we should revisit in a later episode as suicide is often described as an attempt to breakout of the entrapment of life’s pain. I find conceptual discussions about freedom and entrapment quite stimulating.
Host: And then there was the whole discussion about using telehealth to support a person in distress.
Yes Miguel highlighted the importance of proactively thinking things through with the person, the importance of family as well people on the ground who can respond, he mentioned that this was not that different to what would be needed if he was seeing someone face to face.
Host: We also had a very content heavy guest episode with Shazzy Tharby, couple of episodes back, in which Shazzy highlighted the challenges of supporting Autistic people in suicidal distress and how those challenges can be overcome.
Expert: Yes there were lots of practical tips that health professionals can keep in mind, right from first contact like the level of lighting in the consulting room, or the language one uses in everyday practice, asking an autistic person how are you feeling may draw a blank but if we used the Gottman feeling wheel they can clearly articulate how they are feeling.
Host: Interesting thing about the language you had your wrist slapped for saying people with autism.
Expert: Yes, indeed, Shazzy was advocating a person first approach which she said translates into phrases like autistic people, in mental health we have travelled in the other direction where we will be frowned on if used the term schizophrenic, we will say a person with schizophrenia as there is much more to a person’s life than the mental illness. So I have been trying to use the term an autistic person since the podcast recording, and I must say that I find it a bit strange.
Host: Shazzy also talked about the direct exchange from autistic people and how the same principles of collaboration apply to them.
Expert: Yes she highlighted how the straight talking should not be seen as rudeness, that is how they are communicating their distress, and the distress is valid even in the absence of some of the other emotional cues that we often look for. All in all it’s a vital episode and one that you need to listen to as it is so easy to get things wrong. I certainly learnt a lot during that interview.
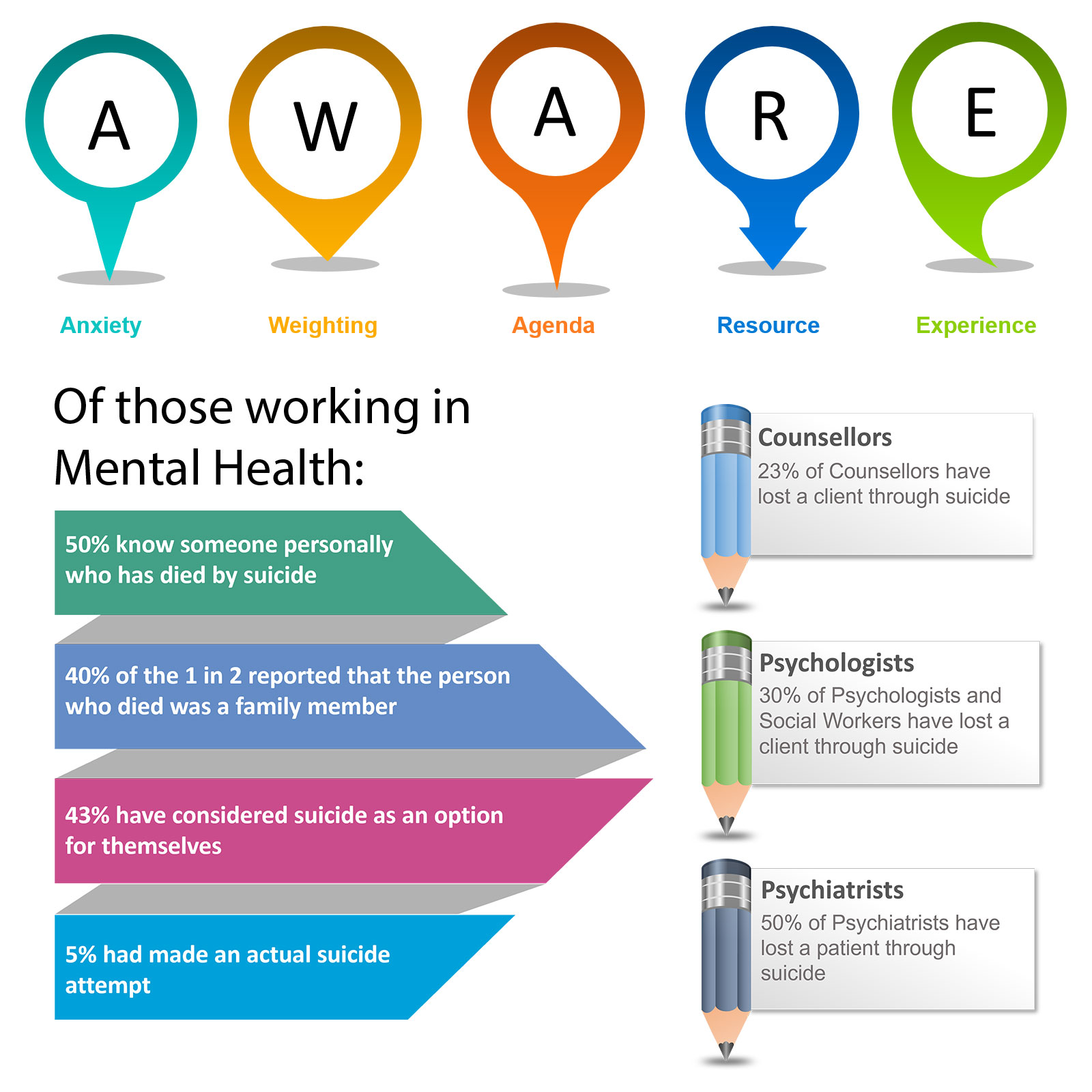
Host: Ok so on to today’s topic, we are on to the last letter of the AWARE acronym, E for experience.
Expert: Yes we are indeed, so A is for anxiety, we discussed how anxiety can get in the way of us properly exploring risk and its impact on decision making. We discussed the two mental spaces, rational and rationalizing. Rational is information first, decision later and rationalizing is decision first followed by selection of information to support the decision or action. This theme plays out in all the AWARE factors. We then explored W for weighting and how much weighting assessors put on certain diagnostic groups namely personality disorder, and substance misuse and how suicidality in these groups often count for less, also how an acute course of illness gets more priority than chronic although those who are chronically unwell may have lost touch with hope and finally how suicidality caused by modifiable social factors are often considered by healthcare staff as outside their core remit of work and these patients end up receiving less support than those with a clear cut biological mental illness. After W was another A for Agenda and we talked about how an assessment get skewed by the agenda that the assessor perceives, this may be in the referrer, patient or family. The next letter R is for resources, whether that be beds or workload in a team and its impact on decision making. We again talked about the two mental spaces, rational and rationalizing, how tempting it is to justify a resource led decision as one that has been taken in the patient’s best interest. Staying in the rational space does not suddenly give us more beds, but we are more aware of the risks involves as we have not rationalized them away thus we might engage in far more stringent safety planning.
Host: That was a quick run through the first four AWARE factors and now to the final one. Experience. DOES YOUR EXPERIENCE HELP OR HINDER?
Expert: The AWARE study showed that the experience of managing a patient previously had a considerable impact on clinical decisions that were made post assessment. Most clinicians found their prior knowledge helpful in deciding what the best course of action ought to be. However it was also apparent that sometimes this past knowledge was used to justify jumping to conclusions and assessments were not as thorough as they ought to be. Presentations and risk are dynamic and prone to change, even if it is the same patient presenting repeatedly in crisis.
Host: Other than that though surely being experienced is a good thing, when a lay person selects a doctor they are often looking for those who are experienced.
Expert: And rightly so, experience by and large is a good thing, the more a professional has seen in terms of breadth of presentations and depth of complexity, the more capable they are in navigating challenging scenarios and circumstances.
Host: So what is the issue?
Expert: The issue arises when experience gets in the way of exploring the unique circumstances of each person’s each presentation.
Host: And this is what you meant by saying assessors jumping to conclusions
Expert: Yes and that too very early in an assessment, it is normal to spot similarities and patterns, that’s how we comprehend the world around us
Host: The way in which a professional generalizes past experience to a current presentation.
Expert: And there are four different ways in which you can think about it, firstly of the same patient at different time points, secondly of different patients but of the same diagnostic groups, then there are different patients that belong to the same demographics and finally different patients from different groups being treated similarly.
Host: Lets work our way through each of them starting with the same patient who presents at different time points, I assuming this applies to group who may repeatedly present in crisis.
Expert: Yes and they may have a well documented acute management plan and there may be very good reasons why a clinician assessing a person who is frequently presenting to ED should stay consistent to the plan that has been agreed on. But sometimes the presentation may have changed, someone who has been chronically suicidal may be presenting in an acute on chronic presentation, like an escalation of self harming from their arms to their neck and face but if too rigidly stick to the plan that has been divsed one may overlook the change in presentation.
Host: Can you provide some statements from the AWARE study
Expert: Sure, quote unquote – “I have nursed her many times over the years, this does not appear to be any different, and believe me once she comes into hospital her behaviour escalates and she regresses every time discharge is mentioned” Statements like this are not uncommon as people use their past knowledge of a person they have cared for to decide what might be the best course of action in the here and now. Many times they are correct but there has to be a degree of cognitive flexibility so that changes in presentation are picked up in frequent presenters. Also one needs to ask that if they are repeatedly presenting whatever is their need is not being met and perhaps more work needs to be done in the community to meet that need or else just turning them away from ED and asking them to follow the plan is setting them up to fail as they will represent as the need, whatever that might be, has not been met.
Host: Ok lets look at the second group – different patients but from the same diagnostic group
Expert: Here is a nice quote from the AWARE study that captures this generalizing sentiment “Half my time is spent in supporting people with borderline personality, I have now learnt the hard way that with them one has to stick to the boundaries and not admit, If they see you being soft you will get sucked in.” Clinicians are known to generalise their learning from one or few patients of a diagnostic group to all patients, loosing the opportunity for person centred care delivery.
Host: This sounds more like an approach or ethos of care delivery to patients of certain diagnostic group.
Expert: Yes and here it might sound like an unhelpful way to treat all patients with borderline personality disorder in this way, but it could be something positive as well like a practitioner feeling and believing that people with borderline personality have had a horrendous past and they should get all the kindness and compassion that there is. The point that we are miking is not that whether experience is right or wrong but that the experience of a diagnostic group influences clinical decisions.
Host: This is similar I assume to different patients from the same demographic population.
Expert: Yes that’s correct, very similar but you are replacing diagnosis with demographics, so here is a quote from a clinician in the AWARE study “The two groups I find difficult are young men into drugs who are not willing to take any responsibility, they just frustrate me, but it is the middle aged middle class depressed agitated men who really scare me since the suicide in the team, they always know what the right thing to say is.” Clinicians will often stereotype a particular demographic due to past experience of things going well or badly wrong.
Host: That is inevitable
Expert: Yes it is, but we need to remain mindful of our beliefs. We did have a middle aged man who took his life while being supported by the crisis team, it came completely out of the blue, in fact the team thought that he was doing so much better and were considering his discharge, and since then positive risk taking for middle aged males took a nose dive. This relates back to anxiety, the first aware factor, not that every middle aged man is risky but the experience of the adverse incident impacting practice and hugely influencing decision making.
Host: And finally experience just being generalized irrespective of similarities or dissimilarities.
Expert: Yes that is captured nicely in this quote “I have got some standard crisis plans that I can draw on for patients who fit the bill.” A crisis plan which might have been designed specifically for a patient might not be suitable for another. These plans need agreement and the support of family, to generalise without that support may be dangerous.
Host: I guess having a framework that one personalizes to the needs of the person is ok, but just using the same plan in a thoughtless fashion is not helpful.
Expert: Yes this is often part of the tick box mindset that emerges in highly pressured environments, no one has the time to think things through, so for example doing things just because they have to be done, take the safety plan of a white middle class male with supportive family and apply that to an indigenous female who may not have any family but has got elders to lean on.
Host: So this is a good example of hitting the target but missing the point. I do want to go back to the experience of suicide, here are some figures
23% of Counsellors have lost a client through suicide
30% of Psychologists and Social Workers have lost a client through suicide
50% of Psychiatrists have lost a patient through suicide
Now that is 1 in 2 psychiatrists and 1 in 3 psychologist and 1 in 4 counsellors, that is significant and perhaps one of the most traumatic things a professional has to come to terms with.
Expert: For those who work in mental health it is often said that there are two groups of professionals, those who have had a suicide and those who are going to have one, this is a very challenging thought and after losing a patient through suicide it influences your decision making, we talked about risk averse clinical care in the Care Compass, where care becomes paternalistic and prescriptive. That has its own problems and has to be mindfully managed in supervision and reflective parctice.
Host: That is loss in the professional context, but there will be those who have had PERSONAL EXPERIENCE OF SUICIDE, does that HELP OR HINDER
Expert: It is inevitable, that decision making or management styles in assessors who have lost someone through suicide or themselves have had their battles with suicidal urges and acts will be influenced by their personal experience.
Host: Yes there is that too, there are some who would have had their own struggles with suicidal thoughts and feelings.
Expert: It does influence decision making, to expect otherwise is unrealistic. However, one has to develop an awareness of how the experience impacts their professional work. It can be positive or negative and it needs to be addressed in a supportive reflective space, either with a mentor or supervisor.
Host: This is reminiscent of the discussion we had regarding attitudes to suicide.
Expert: That’s correct. In particular understanding how one talks about suicide with patients, how one personally relates, how much of their personal experience does one share, what actions does one take or doesn’t can be protective both for the person being supported and the professional’s practice.
Host: What do you do if there are areas of concerns?
Expert: Well they need to be actively addressed so no harm comes to patients. A professional’s past might provide a sense of deep empathy for the person’s present distress, however the same past could intrude and take over interfering with present effectiveness. If a professional’s present is a daily personal struggle with suicidally caution has to be exercised and fitness to practice procedures should be considered.
Host: Do you have any suggestions for those professionals who find it difficult to strike that balance.
Expert: I think reading personal narratives and memoirs can be quite enlightening. Consider reading An Unquiet Mind: A Memoir of Moods and Madness by Kay Jamison and Cracked, Not Broken: Surviving and Thriving after a Suicide Attempt by Kevin Hines.
Host: Sounds like on the POSITIVE side there is going to be Empathy and on the NEGATIVE side there may be Over Identification
Expert: Yes, people with a personal experience of suicide will bring keen insight into what it feels like to walk in the shoes of a person who is suicidal. Feeling that someone really does understand their psychological pain can be quite protective, this is the foundation of relational safety. But as you pointed out, lived experience can result in over identification leading to taking on a saviour role with rescue fantasies. In some this may result in boundary violations. In others their personal experience may be so painful that they avoid talking about suicide resulting in an unsafe situation.
Host: In short PROFESSIONAL’s EXPERIENCE OF SUICIDE both in the person and professional sphere MAY HELP OR HINDER. Here are some facts to consider;
50% of those in mental health care know someone personally who has died by suicide1
40% of the 1 in 2 reported that the person who died was a family member1
43% have considered suicide as an option for themselves 2
5% had made an actual suicide attempt2
Expert: As you can tell from those numbers this is not a rarity, so it deserves our attention, the overidentification does not just cause rescue fantasies and sometimes boundary violations, for some practitioners they freeze and have outright impairment, limiting their ability to ask or talk about suicide. It is really important that such anxieties are picked up in supervision and discussed candidly. Also there is the need skills building in helping professionals connect with empathy, drawing on their own lived experience without making the dialogue about their own loss. These are nuanced skills and it is crucial that professionals get support for them.
Host: This brings us to the end of episode 18. Last but not the least we have covered a very important AWARE factor today, experience, whether that be just the experience of assessing and caring for people in suicidal distress and generalising that exposure to future patients or the professional or personal experience of losing a patient or loved one to suicide. Remember the show notes and images will be at the blog on www.progress.guide and you can get the PROTECT suicide prevention Guidebook from Amazon. There are number of online video courses as well. Pause and think which groups of patients you find challenging. In the recent past which patient had kept you awake at night and why? When it comes to such patients are there particular trigger points for you that bring out a specific response in terms of your risk taking or decision making. Have you lost anyone, patient or a loved one to suicide? Have you had support for that loss? Do spend some time reflecting and looking in the rear view mirror. Reflection is an essential element of progress to practice. Share your musings with us. Tweet your thoughts about experience of or lack of and tag #GuideProgress. It helps get the word out about the podcast to more professionals. You can email your thoughts to us at admin@progress.guide with your suggestions and comments particularly if you have questions and want us to cover certain topics in the discussion. In the next episode, we will build on the discussion regarding experience with a phenomenon called Creep Crash Crawl as we ran out of time today. Please spread the word, you can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Helping healthcare professionals become aware of their decision making processes is an essential step in creating a workforce that is self-aware. Remember together we can make a difference. Tune in next Friday and we will discuss how risk taking in a professional who is regularly exposed to suicidality evolves over time and how it impacts their practice. Thank you for joining us today and keep spreading the word.
You may also like
19 | Creep Crash Crawl
G4 | Dr Miguel de Seixas ~ From Vietnam with Love

