13 | Introducing ASSESS and Attitudes to Suicide
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date April 15, 2022
Transcript
Host: Good day, This is Mahi, your host, we are on to episode 13 and about to begin the ASSESS module. In episode 11 we did a summary of the CORE module and in episode 12 we elaborated on the key mindset shift from top to TAP and the progress to practice that shift will bring. Manaan provided the rationale for moving from prediction to prevention, rebalancing the focus on the past with the present and ensuring that we look beyond the deficits in the person and help them reconnect with their assets, their strengths. If you haven’t listened to episodes 11 and 12, now might be a good time to do so but if you just want to dive in to the ASSESS module, do remember that progress to practice will come from the 3 shifts: prediction to prevention, past to future and deficits to assets. As usual for the key messages and for the messages in images either go to the podcast blog at www.progress.guide or you can get the PROTECT Guidebook from Amazon to read along. The images are particularly helpful for visual learners and help with retention. Ok let’s get started with the 2nd module ASSESS. Manaan, I noticed that just like CORE, ASSESS too is an acronym. Making up acronyms seems to be your favourite pass time.
Expert: You can say that again, yes there are quite a few acronyms, sometimes I feel a few too many, however as you were saying retention is critical. Health professionals hold so much data and information in their head, whenever I run my advanced courses, the days are pretty full on, there is concept after concept and in between these concepts there are the experiential exercises where I am expecting professionals who have just learn a concept to practice them with a partner. Although we looked at quite a few practical applications of the key concepts in CORE, in essence it was theoretical. ASSESS and ASPIRE is very practical. One of the things that helps with rapid translation from factual knowledge into practice is a simple acronym that helps professionals retain the key steps and not miss out key issues to be addressed or resolved.
Host: And some of the acronyms are just to provide a structure to the course.
Expert: Yes, that’s correct, they are meant for the Progress Guides, i.e. trainers, the 3 modules, CORE, ASSESS and ASPIRE are all acronyms but professionals don’t have to remember them, it helps the people who are running the course, to progress from one chapter to the other.
Host: ASSESS has 6 letters, that would mean 6 chapters
Expert: That is correct, the module follows a logical structure and begins with an attempt to get a deeper understanding of oneself, followed by the different actions in the assessment sequence. We then take a look at suicide phenomenology, attempting to understand progression from one level to another, as well as techniques and strategies for interactions, all the way to formulation and documentation.
Host: Looking at the guidebook, the first chapter is Appraise Decision.
Expert: Yes, for mental health professionals to continue to grow as an assessor it is vital for them to be self – AWARE. In this chapter we help professionals get a deeper understanding of the key factors that influence their clinical decisions.
Host: This has the acronym AWARE
Expert: Yes, AWARE is a nice word for the acronym as we are trying to make the implicit explicit. The acronym covers the five groups of factors that morph our decisions and a lot of the time we are not even conscious of how subtle influence can changed the trajectory of our assessment and the decisions we make.
Host: This is followed by sequence of actions.
Expert: Here we have the acronym AIMS, standing for assessment, intervention, monitoring, step up or step down. That’s an overview of the actions but we do get into the nitty gritty of the different parts of the assessment itself and how much time one allocates to each action and is the balance correct.
Host: Then on to Suicidal Presentation
Expert: We explore the phenomenology of suicidal distress using the STEPS model which is purpose built to track suicidality as it evolves in individuals.
Host: Looking at the guidebook, this seems to be quite a detailed chapter
Expert: Yes, we begin with Emil Durkheim’s model in 1897 and make our way to the most contemporary ideation to action models. We also get more nuanced in our understanding of risk.
Host: You mean static and dynamic factors
Expert: Well, we go a step further and divide up static factors into static i.e. zero flux and stable, some but limited change taking months to years and dynamic factors get divided into dynamic, change over days to weeks and fluid factors that may influence changes hourly
Host: There is also a section on acute and chronic risk
Expert: Yes, we help people differentiate out their approach and response based on whether the risk is acute or chronic and acute on chronic. Vital in people with borderline personality disorder, something that many professionals struggle with. We also teach rapid assessment techniques with four vital areas of information that help with the formulation.
Host: I guess we are moving on to Empathic interaction
Expert: Yes, the foundation of the STEPS model leads to this model called B4Now, well the full name should be 1-2-3-B4-Now as we systematically work our way through day 1, last 2 weeks, last 3 months, before this episode and the here and now looking ahead.
Host: Is this where you also teach the validity techniques and the narrative method
Expert: Yes, Shea’s validity techniques bring with them significant focus and intentionality where as the narrative method helps the person articulate their story, feel listened to and get validated. One provides focused data the other provides the narrative and you need both for a good formulation. B4Now is our attempt to synthesise the two approaches meeting the need in the assessor to get all the necessary data and meeting the need in the suicidal person to be heard and listened to.
Host: This then gives rise to the Safety Formulation
Expert: This is a key skill for an assessor to synthesise all the information they have collated so that they can make mindful decisions and take mindful action.
Host: You use the DESPAIR acronym
Expert: Yes the term DESPIAR brings together all the key pieces of information that research has shown is of vital importance in risk management. The reason why DESPAIR is vital in terms of safe practice will become clearer when we go through the AWARE framework. DESPAIR helps us consider all the information that is valid and not just focus in on pieces of information that will justify our decision or action.
Host: And the final chapter in the ASSESS module is Safety Documentation
Expert: Another memorable acronym here called NOTES where we build on the Safety formulation of DESPAIR and help the professional engage in paperwork for proper work, help them appraise their options for action and mindfully document why they chose which option for therapeutic intervention along with an escalation plan and the people they are sharing the information with.
Host: So, in terms of sharing you mean the people in the person’s life, does that bring us back to relational safety.
Expert: Yes, it does, safety is created through a partnership, not just the partnership between the professional and the person in distress but their entire natural circles of support as well as professional, and often who the information is shared with can make or break the journey to safety, healing or recovery, but we will discuss that in detail when we do NOTES.
Host: That’s a great overview of the ASSESS module, A is for Appraise decisions, S is for Sequence of actions, the next S is for Suicidal Presentation, E is for Empathic interaction, S is for Safety formulation and the final S is for Safety Documentation. And going through these chapters you will learn about the AWARE and AIMS frameworks, the STEPS model, the B4Now technique and the DESPAIR and NOTES framework.
Expert: I could not have said it better myself.
Host: We have some time today, shall we get started with the 1st chapter from ASSESS
Expert: Why not, that would be appraising decisions
Host: So, given we have some time but not a lot, we could take a look at something specific, like attitudes to suicide and suicidal distress.
Expert: That is a good starting point as the attitudes we hold have a significant influence in the way in which we interact with people in suicidal distress as well as the decisions we make.
Host: How shall we do this, in the courses you conduct, you tend to do this part as a silent reflective exercise before a group discussion.
Expert: Our podcast listeners can always hit the pause button to think after each question, or listen to some of the questions together and then hit pause to think about them. The important thing is to conduct an honest examination.
Host: You mentioned that attitudes influence decisions, could you give a concrete example so our listeners can understand why this is so important.
Expert: It is well established that attitudes towards suicide influence behaviours in the professional sphere, and there is a spectrum for these beliefs, for example a practitioner who considers suicide to be unequivocally wrong may come across as judgemental and the one who considers it permissible may fail to take definitive action. In many smaller ways, a professional stance towards suicide prevention can disrupt treatment.
Host: So are there right and wrong attitudes
Expert: There are no right or wrong attitudes; the goal of the reflective exercise is to prompt a journey of self-discovery that can help modulate one’s own responses towards people in suicidal distress.
Host: So, let’s have some of the reflective questions
Expert: Ok, let’s begin with should suicide always be prevented. Why or why not?
Host: Isn’t that quite simple, surely health professionals are duty bound to do whatever is needed to prevent suicide.
Expert: But that is not the question, the question is should suicide always be prevented. Even for a health professional under that veneer of simplicity is a degree of complexity. As a doctor I have taken the Hippocratic Oath to uphold specific ethical standards. The phrase first do no harm, what does it actually mean in terms of prolonging life with excruciating pain in our case emotional pain and suffering. Clearly if there is a cause that can be treated and there is the hope of recovery, life is worth fighting for, but if there is no hope or it is a terminal condition, then who are we to prolong pain and suffering and preventing a person to die with dignity. I am not saying this is my position, I am just opening up a can of worms to consider.
Host: So, it is not as straight forward as I thought.
Expert: And there are no right or wrong answers, just becoming aware of one’s position, where do you stand, if you are struggling with it, it is worth thinking about under what circumstances will you consider suicide for yourself (if at all)? Making it up close and personal might give you a fairly good idea about your stance.
Host: That is a tough one, I can see what you meant by if there is no hope and the condition is terminal why someone might think why continue with this pain and suffering.
Expert: This is then a good time to think about what do you think about people who attempt suicide or die by it? What feelings do they generate in you?
Host: I guess this relates back to whether one thinks of suicide as unequivocally wrong or that suicide should be a permissible act.
Expert: Yes, if you think it is unequivocally wrong then you will have difficulty listening nonjudgmentally to a person describing compelling reasons to die by suicide and have difficulty forming an empathic therapeutic alliance and intent is withheld.
Host: And if you think it is a permissible act?
Expert: Then as I said earlier you may not take definitive actions to thwart a person’s suicidal urges or plans, this might lead to an avoidable tragedy and care provided might be considered negligent
Host: So, attitudes are quite important
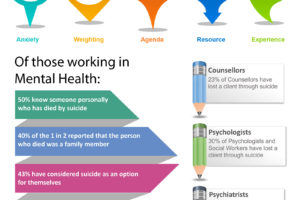
Expert: Mental health professionals need to have a solid understanding of their attitudes towards suicide and suicidal behaviour. The other common one to be aware of is whether they consider suicide to be a sin or a right, their stance can negatively influence assessment and treatment, even outside of their awareness.
Host: I guess whatever one’s beliefs, it is true that the major world religions once condemned suicide universally.
Expert: Yes, but most now make allowances for suicide that occurs because of mental illness or impairment. In many countries a suicide attempt was considered an illegal act till recently.
Host: I remember discussing in a previous episode about how I had empathy for some who might think that suicide is a selfish act, like a suicide that leaves behind a widow with 3 young children, or a suicide in a teacher who is much loved his students that affects a whole school.
Expert: Yes, one can see why people might think that the person is selfish for scarring young minds or leaving behind a widow with young children. However, almost always, people who die by suicide do so under the influence of mental illness, hopelessness, trauma, pain, or some other seemingly impossible problem. It is questionable whether the person is to blame for actions that generally forces them beyond their control. The psychologist Thomas Joiner also disputes the notion of selfishness by pointing out that many people who attempt or die by suicide actually want to help the people they love, not hurt them. Falling for the lies of depression, hopelessness or other mental pain, they often believe mostly to the astonishment of their family and friends that the suicide will make life easier for them. However misguided might be the wish to spare others is hardly selfish.
Host: What you are saying is in their mind they are being selfless rather than selfish.
Expert: Yes, it is the lens through which you view it, another common one to think about is, is Suicide cowardice or Suicide takes courage. Some people view suicide as taking the easy way out. Others note that it requires courage to overcome the survival instinct and actually end one’s life.
Host: Essentially you are saying that mental health professionals need to have a solid understanding of their attitudes towards suicide and suicidal behaviour.
Expert: Beliefs harboured by mental health professionals are spread across the spectrum. The dichotomies above are some of the common ones that can jump-start an honest examination of one’s suicide-related belief. Pause and think about your attitude towards suicide: many in mental health care hold a firm belief that suicide is not an option, not only is this unempathic for the person in severe psychological pain, it simply is not true, every day 8 Australians take their life by suicide, we may not like it, we may not morally approve, we are clinically opposed, but the fact is that a determined person who means to die can achieve this goal through suicide, so we considering it an option or not is irrelevant. I am assuming that no one is under the illusion that we can lock people up till a suicidal person shows clinical stability, even if we magically quadrupled our beds this would not be possible and who claims that an inpatient environment is immune to suicide. The sooner we understand our own attitudes to suicide and grapple with it the more effectively will we respond to the psychological pain which is at the root of suicidal distress. The hope is that clinicians become mindful of how their views on suicide prevention affect how they respond to a suicidal person. This will prompt them to take necessary safeguards so that the care they provide is the most effective and ethical.
Host: You are asking people to Stop or at least Pause, you have made 3 key points
- Attitudes towards suicide influence decisions
- Attitudes towards suicide influence rapport and empathy
- Attitudes towards suicide influence care and support we offer
Expert: Once you have got that foundation, Reflect and Rewind
- Recognise your attitudes
- Recognise how these might have influenced decisions and care you have provided
- Engage in open, candid discussion within your team, be prepared to learn from the past
And then you can start and Play forward cause you will recognise if your attitudes are adversely influencing care provision, you need to seek help, consider:
- Personal therapy
- Additional supervision
- Monitor through ongoing reflective practice
Host: This brings us to the end of episode 13, today you have received an overview of all that is there to look forward in the ASSESS module, 6 chapters packed with contemporary knowledge that is designed to bring progress to your practice. We then dived deep into attitudes towards suicide, What do you think about them, where do you stand, is suicide unequivocally wrong, or should it be a permissible act, is it a sin or is it a right, is it selfish or selfless, does it take courage or is it cowardice. No right or wrong attitudes just awareness, awareness that may influence your practice and clinical decisions? We would love to hear from you. Tweet your thoughts about attitudes to suicide at #GuidePorgress. It helps get the word out about the podcast to more professionals and challenge the stigma related to suicide and mental health challenges. You can email your thoughts to us at admin@progress.guide with your suggestions and comments particularly if you have questions and want us to cover certain topics in the discussion. In the next episode, we will introduce the AWARE framework and the two mental spaces, rational and rationalising, knowledge that will transform your practice. You can access all the information at www.progress.guide. You can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Helping healthcare professionals become aware of their attitudes to suicide is an essential step in creating a workforce that is self-aware. Remember together we can make a difference. Tune in next Friday and we will dive into the AWARE framework. Thank you for joining us today and keep spreading the word.
Previous post
G2 | Dr Stan Steindl on Navigating Suicidal Ambivalence Using Motivational Interviewing
You may also like

19 | Creep Crash Crawl
18 | AWARE 5 – Experience