12 | Progress to Practice – 3 Key Shifts in Crisis Care
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date April 1, 2022
Episode 12 - Progress to Practice
Host: Hope you are having a wonderful day, This is Mahi, your host, we are on to episode 12. In episode 11 we did a summary of the CORE module. Hope that will help retain some of the key messages and for the messages in images either go to the podcast blog at www.progress.guide or you can get the PROTECT Guidebook from Amazon to read along. The images are particularly helpful for visual learners and help with retention. Manaan, you ended the previous episode on a mysterious note, wanting to hold on to the discussion about top to TAP for the next episode saying something about a new training program called 7 SAFE Steps. Are you about to shed light on what’s in the pipeline.
Expert: Yes, I am indeed and I am very excited about it. 7 SAFE Steps is a new training program for 2022. Put simply it is a sequence of 7 conversations, version 1 is geared towards inpatient staff, providing them the skills and competencies they need to connect with compassion and create safety through human connection, not just safety on the ward but also in the community as the person navigates the tricky transition back out dealing with the problems with which they originally came in, a time that we know is extremely risky.
Host: You really sound very excited about it.
Expert: I am, cause it is the best training program ever.
Host: But you say that about every course you design.
Expert: That is true, I am often asked which is my favourite course, and it is always the one that I am working on. But that is how it should be, I will not be putting something out to students if I felt this was not my best work, keep working on it till it is my best work and this one is special, the conversations we have designed have one goal in mind. It is to convey: “What lies ahead of you & what lies behind you is nothing compared to what lies within you.”
Host: That’s your hero, Mahatma Gandhi
Expert: Well these specific words are attributed to him, but Ralph Waldo Emerson, the American Essayist said something very similar “What lies behind you and what lies in front of you, pales in comparison to what lies inside of you.” Irrespective of who said it I love the idea of helping people reconnect with their strengths, their agency, their assets and in the process generate hope for today and tomorrows that are yet to come.
Goal: Create Relational Safety
Host: and that is the essence of Relational Safety.
Expert: Exactly, relational Safety arises within a scaffolding of a deeply empathic therapeutic alliance, an alliance that is based on mutual respect, genuine curiosity, and a true acknowledgement of the overwhelming emotional suffering. Each of the 7 conversations, aspires to create the human connection of hope and healing, creating safety in the present and the future.
Host: So 7 SAFE Steps is based on the PROTECT framework
Expert: Yes it is, but we have taken complex concepts and simplified them into pragmatic conversations, its the translation from theory to praxis that has been reinvigorating, Its innovative, interactive and intuitive in its design and delivery and above all creates time and space for professionals who work in settings that are like pressure cookers to pause and think: What in my current practice might limit my ability to fully realize the potential of the relationship that I am about to form with a person in suicidal distress?
Host: I can see what you are getting at and why you have been saving the top to TAP discussion. In the experiential exercises of the PROTECT workbook you repeatedly attempt to drive home how practice is often dictated by mindsets we hold, and the answers to progress to practice might lie hidden there.
The Key Mindset Shift: TOP to TAP
Mindsets shape interactions:
Expert: You really are developing the superpower of mind reading. Yes, clinical practice is akin to an iceberg. Only 3/10th is above the water; this is what we see and address. But the invisible 7/10th, the sum of our beliefs, values, needs, both met and unmet, has a significant impact on how we behave and interact with a person in suicidal distress.
Host: That’s what we call a mindset, you learnt this in episode 8 when Manaan talked about Sir Roger Bannister and the four minute mile. They are the paradigms through which we make sense of the world.
Expert: Our mindsets dictate how we behave in the clinical sphere and how we deliver care. If you have been listening to the podcast you will know that we believe that the key to unlocking the potential of the relationship involves a shift in the professional’s mindset of being the sole expert, the professional needs to move from a position of power, where they are the source of knowledge and expertise, to one where they are partners in an enabling role, supporting the person to reconnect with hope and their strengths. The clinician brings professional expertise and the person in distress brings their unique lived experience.
Host: So to summarise, for the magic of Relational Safety to happen a shift in the professional’s position from TOP to TAP is needed.
Expert: and If such a shift were to happen, Progress to Practice will be an automatic consequence, I am going outline 3 shifts in practice that are absolutely fundamental, they have gone into the design of 7 SAFE Steps but are also critical in you coming to grips with the ASSESS and ASPIRE module.
Host: For those who don’t know, Progress to Practice is our slogan at Progress Guide, in fact Manaan ends every training session with the one key Progress to Practice that the new knowledge or skill will bring.
Expert: Passion to Purpose, Progress to Practice, pretty much sums up our mission and vision and gives us our direction of travel. So if you can embrace top to TAP you will make the 3 shifts in practice, the first is you will move from the practice of prediction to one of prevention, the second is you will rebalance your focus on the past and move towards the future and most importantly you will move from a deficits approach to one that is assets based.
Host: prediction to prevention, past to future and deficits to assets, were you planning to explore each one of them.
Expert: Absolutely, they are critical to what lies ahead in the future episodes and we will return to them repeatedly.

The 3 Key Shifts in Practice:
Prediction to Prevention:
Host: Ok, let’s begin with prediction to prevention
Expert: The practice of prediction involves risk categorisation into low, medium and high. The clinician attempts to answer “how much of a risk does the person pose to themselves”. This approach identifies the person as the problem to be fixed and minimises all the potential that the person has.
Host: Not only does it undermine the partnership approach needed for relational safety, you outlined in episode 6 and 7 the evidence for the futility of risk categorisation.
Expert: Yes, there is significant evidence to suggest that empirical risk factor based prediction is flawed. It has minimal impact on individual outcomes for patients, the National Confidential Inquiry data show that every year and after 50 years of research and practice based on risk factors, overall suicide rates haven’t changed. High, Medium, Low risk stratification is a static way of assessing risk that is inherently dynamic and multifactorial in nature.
Host: Given you mentioned that version 1 of 7 SAFE Steps was for inpatient professionals, will you agree that within the confines of an inpatient setting, the risk is less dynamic and may be well contained as professionals may be able to address the risk variables.
Expert: To an extent, as professionals are around 24-7, but even then things can change rapidly, in the western world organisations have been trying to make inpatient suicide a never event for over a decade but still it happens. But it is true that your ability to influence the risk is greater. However, an inpatient ward is not the real world. The goal of an inpatient stay is to prepare the person for life outside. And the moment one is discharged, not only do the variables multiply manyfold, but they also now have to navigate the challenges with which they originally presented at admission.
Host: So at discharge the static categorical prediction of high, medium, low on the ward becomes redundant.
Expert: Exactly, in 7 SAFE STEPS and ASSESS and ASPIRE we promote a mindset of prevention. This assumes that a person whose mental health challenges have been such, that they have needed an inpatient stay, life circumstances may rapidly conspire for them in a way that they may end up posing a risk to self.
Host: Does this assumption hold irrespective of their primary presenting problem, which may not include suicidal distress.
Expert: Absolutely, the data shows over and over again that over 80% of people are classed as low risk at last contact. If they have made it on to a psychiatric ward or are in secondary care mental health services for that matter, life circumstances can change fairly abruptly to go from no or little risk to posing clear and imminent danger to oneself. So do not waste your time predicting, embrace prevention instead for everyone in secondary care settings. A mindset of prevention attempts to establish a partnership within which one may explore “what are the challenging circumstances ahead and what can be done about them?”
Host: This is very different to prediction where the thought process may stop once someone is rated as at low risk.
Expert: We know risk is dynamic, and unless you are looking with a lens of prevention you will not be preparing for future adversities.
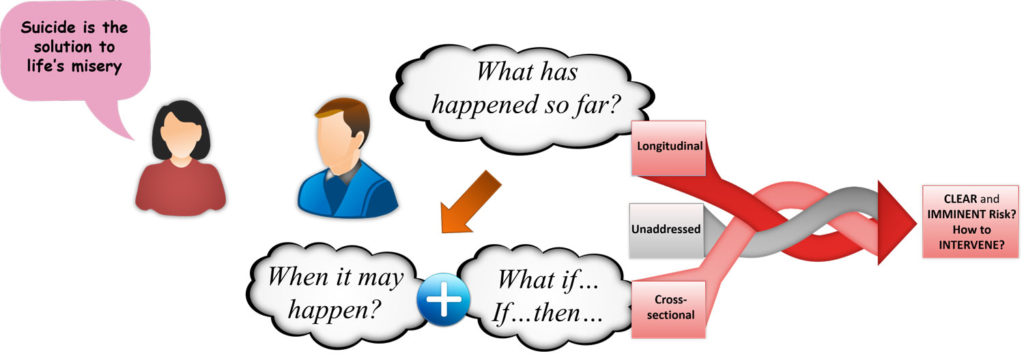
Past to Future:
Host: This seems like a nice segue way to the next practice change, past to future.
Expert: Prevention is a future focused activity. But most risk assessments focus on the past and do not attend with similar rigour to future adversities,
Host: But who knows the future, as you have been saying risk is multifactorial and complex.
Expert: True, some of the risk is unpredictable, but for most people there is a hell of a lot of predictable risk. Often it is the very circumstances with which they have presented in crisis or the predictability lies in the source of their emotional pain.
Host: In your training programs, often, you use Louis Pasteur’s words chance favours the prepared mind.
Expert: Actually, that is a very strong theme in 7 SAFE STEPS, chance favours the prepared mind, particularly in conversation 3 and 4. To answer the prevention question (what are the challenging circumstances ahead and what can be done about them?), a rebalancing of emphasis from the past to the future is needed.
Host: But it is also important to look at the past
Expert: Yes past does predict future behaviour, that’s why we teach many techniques to explore the past like the B4Now technique, pattern mapping etc, but is the time distribution in the assessment reflective of a prevention mindset? How much of the assessment do we spend on the past and how much on the future working with the person and their family on safety planning and addressing risk.
Host: Not in an explicit way but you did touch on some of this in Risk Rethink.
Expert: Yes I did, the backward focus will inform a professional’s opinion on longitudinal risk (how has the risk ebbed and flowed over time, where are we comparted to the baseline or the worst point), but really it is only after grappling with the risk that is left unaddressed post-safety planning that one can comment on crosssectional risk (how does the risk for this person compare to the risk in different patient populations, like patients who are inpatients or in Acute Care Team or in Community Mental Health Team). That is what informs treatment decisions regarding what (intervention) should be delivered where (setting).
Host: What you are saying is professionals need to spend a significant chunk of assessment time looking at the immediate future if they want to make safety planning meaningful.
Expert: Yes, forward focused treatment decisions are vital for prevention and demand a shift in focus from the past to the future. It is the future where we expect the person to rise to the challenges, so please explore it properly.
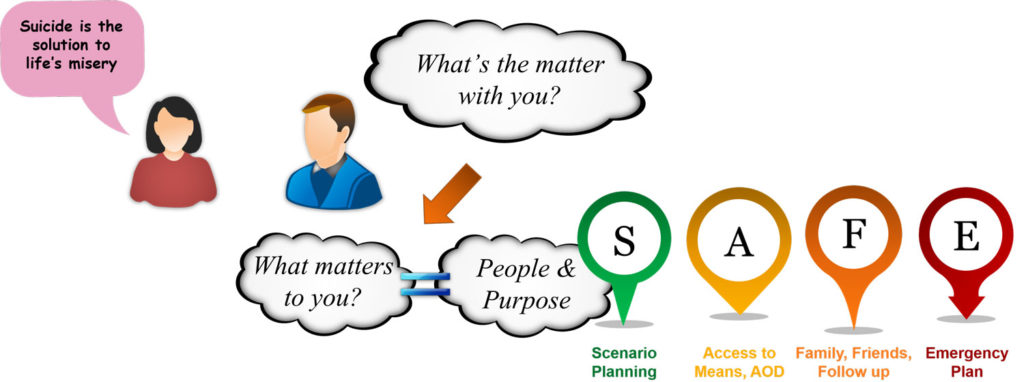
Deficits to Assets:
Host: Rising to the challenge, this calls on the person’s strengths and their natural circle of support, which moves us to the third shift, deficits to assets.
Expert: Perhaps the most important of the three, from the position of top everything seems like a deficit and it is so easy to miss all the assets. Maintaining safety is a shared responsibility and you have to draw on the person’s strengths to maintain it.
Host: In an inpatient setting though, if the risk warrants, it is possible for professionals to take carriage of safety temporarily. Like putting people on continuous engagement or an observation schedule.
Expert: Yes you can, but every time a continuous engagement is initiated there is less staffing resource left for the rest of the patients, so there is an opportunity cost. You cannot just magic more staff out of thin air. And even on a ward with a good staffing complement of a 1 to 4 nursing ratio, most patients, majority of the time are on their own.
Host: And of course you mentioned that the purpose of an inpatient stay is to prepare people for life back in the community.
Expert: That’s correct, the multifactorial and dynamic nature of risk means, that risk may fluctuate incredibly rapidly in the community. Even for those who are getting weekly follow up, 167 of 168 hours in a week, the professional is not with them. The person has to draw on their strengths and their natural circle of support to stay safe.
Host: In essence you are saying that a professional can only do so much in the community.
Expert: And that is not to wash off the responsibility professionals have, they have to prepare the person to stay safe, so a responsibility is there but as professionals we also need to have the humility to understand the limitations of our role in maintaining safety and accept how dependent we are on the person themselves. Staying connected with one’s strengths and coping strategies is paramount, but the conventional assessment and treatment focus is quite heavily on deficits.
Host: As you keep saying a deficit mindset attempts to establish “what’s the matter with you.”
Expert: And an assets mindset is keen to understand “what matters to you.” People do not get suicidal over things that do not matter to them. If one could get an understanding of what mattered to them, they will automatically get an understanding of what’s the matter with them. The former helps us chip away at the cause, the latter in terms of symptoms and diagnosis are only a consequence of the cause.
Host: In 7 SAFE Steps do you focus on this, cause inpatient settings are often very focused on the illness, just because how unwell people are when they get hospitalised.
Expert: This is a major focus, in fact, what matters to me is conversation 1. Patients report time and time again as to how when they walk through the doors of an inpatient setting their identity is stripped away from them, they are no longer a spouse, father, mother, brother, sister, son or daughter, they are no longer a software engineer or a business man or a taxi driver, or for that matter a musician or a cricketer, they become a patient.
Host: Losing one’s identity must feed into the helplessness and hopelessness people perceive when unwell.
Expert: So true, It is what makes peoples life purposeful and meaningful that maintains hope and maintains the ideation to action divide. So, establishing what matters is crucial for safety and recovery. We need to pause and ask, how much of our assessment is focused on eliciting the person’s strengths and do we take the time to highlight their natural circle of support, cause that is the foundation of effective safety planning.
Host: So, if the focus on strengths is minimal, a practice change is warranted.
Expert: Absolutely, and you know what, assets based practice is a highly nuanced skill, too much of it, the person may feel invalidated, and one may come across as attempting to silver line the person’s immensely difficult situation, trivialising their pain. Too little leaves the person helpless and hopeless with the professional holding the responsibility for safety, a responsibility that they cannot fulfil in a meaningful way unless they take an enabling strengths based approach.
Host: This has been an enlightening discussion. Do you want to summarise for our listeners the key messages.
Expert: Firstly, remember in the community the person will be on their own, and to keep the future safe they will have to draw on their own strengths and their natural circle of support. This means that in every interaction particularly during an inpatient stay, professionals have a responsibility to reconnect them with the strengths they possess. Thus time needs to be spent on assets not just deficits. All of this safety that we are trying to create is in the future, so ensure that your assessment is not just one of the past but does justice to future adversities. Remember, chance favours the prepared mind. In this approach lies the foundation of prevention, predicting high, medium, low is a fool’s errand, embrace prevention instead and do not allow any predictions of low risk to create a veneer of safety, look into the future, draw on the person’s strengths and collaboratively work towards hope and healing. Convey through your actions that you have made the move from top to TAP, cause if you have you will value their assets and walk the talk, role modelling “What lies ahead of you & what lies behind you is nothing compared to what lies within you.”
Host: This brings us to the end of episode 12, you have learnt about the 3 practice shifts that stem from top to TAP, Prediction to Prevention, Past to Future and Deficits to Assets. What do you think about them, what are the challenges you foresee in putting them into practice? We would love to hear from you. Tweet your thoughts at #GuidePorgress. It helps get the word out about the podcast to more professionals. You can email us at admin@progress.guide with your suggestions and comments particularly if you have questions and want us to cover certain topics in the discussion. If you would want to know more about 7 SAFE STEPS and how it can be rolled out in your inpatient ward, contact us. In the next episode, we will introduce the different chapters of the ASSESS module and also look at attitudes to suicide which may influence the assessment and interventions we deliver. You can access all the information at www.progress.guide. You can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Providing healthcare professionals contemporary knowledge about how to connect and create relational safety is crucial in suicide prevention. Remember together we can make a difference. Tune in next Friday and we will dive into the ASSESS module. Thank you for joining us today and keep spreading the word.
Next post
G2 | Dr Stan Steindl on Navigating Suicidal Ambivalence Using Motivational Interviewing
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience