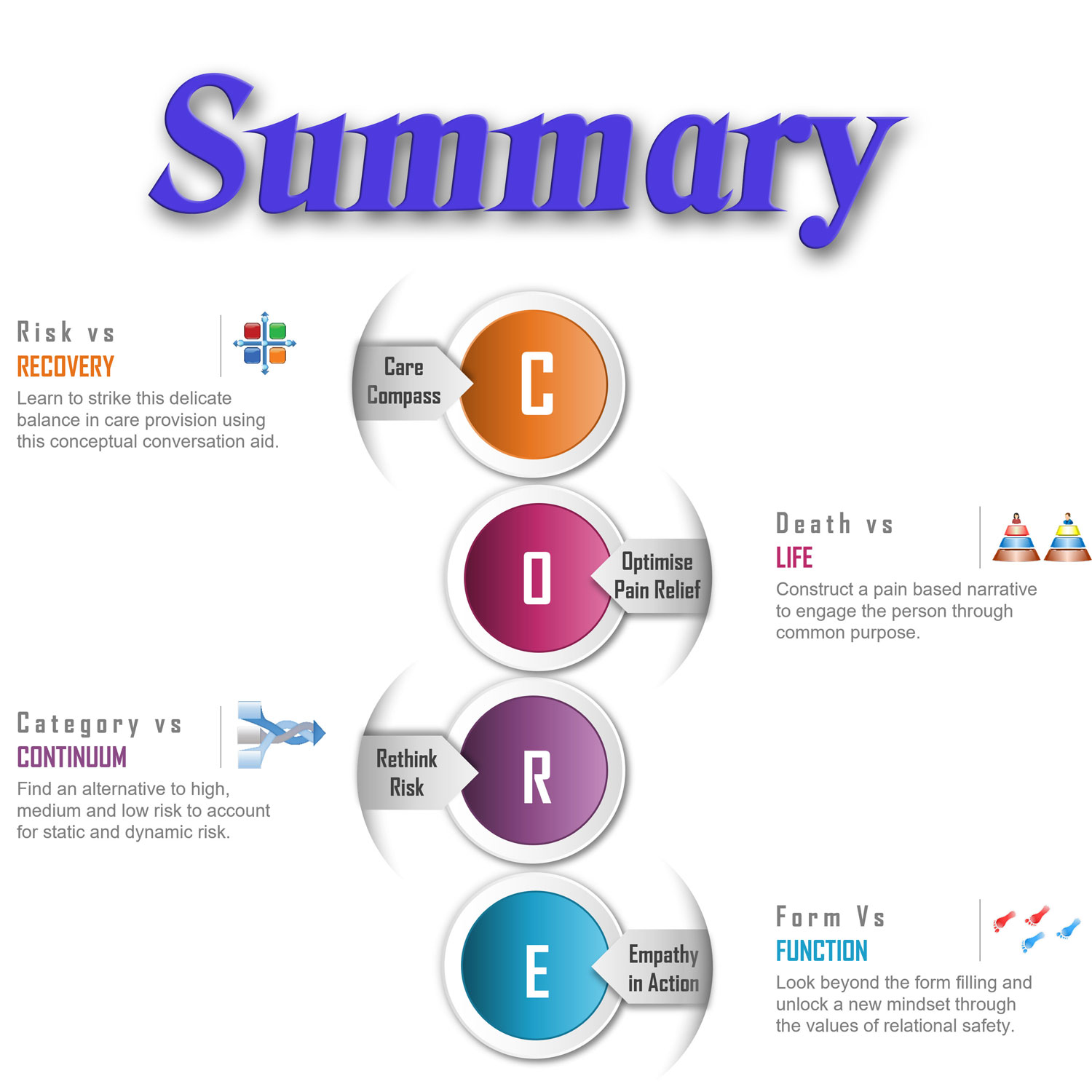
11 | CORE Summary
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date March 18, 2022
Transcript - Episode 11 with the Messages in Images
Host: Good day, I am Mahi, your host, this is episode 11. The first 10 episodes took us through the four chapters of the CORE module. Manaan often acts like a broken record saying protect the CORE, progress all else, meaning retain the CORE in its entirety, it is the solid foundation for the 2 remaining modules ASSESS and ASPIRE, maintaining the CORE in its original allows practitioners to retain the fidelity of the golden thread of relational safety, so new research and development can be smoothly incorporated into ASSESS and ASPIRE. This way PROTECT will continue to progress as the field of suicide prevention evolves. As usual the transcript and the media will be on the blog at www.progress.guide or you can get the PROTECT Guidebook and Workbook from Amazon to read along. So Manaan, what’s on the menu today.
Expert: I was thinking we should do a recap of all the episodes so far. Repetition aids retention, allows us to consolidate the learning, of course nothing helps integrate knowledge into practice more than doing. So please put the knowledge you have gained so far into practice and see how you get along. Reflect on it, ask your selves two simple questions, what worked well and even better if.
Host: I have got a list of the episodes, did you want to start with a recap of the key messages from each episode.
Expert: I think that is time well spent, also I am thinking if a listener has not listened to the first 10 they can still get a sense of the CORE module by listening to this episode which will mean the next module ASSESS will make more sense. Of course we want them to make the time and listen to all the episodes but a summary will help everyone.
Host: OK lets get started in episode 1 you shared your personal narrative and introduced PROTECT and the concept of relational safety.
Expert: Yes, I lost a loved one to suicide and that has been a guiding force for me. I draw a lot of my passion from that early experience. I was a very young doctor at that time. I have written about it on the inside cover of my book and I finish that page with four lines from one of my favourite poets, Emily Dickinson.
Host: Well here we are not constrained for space so you do not have to limit yourselves to the four lines, and its not a long poem anyway, do you want to share it with our listeners?
Expert: sure
Hope is the thing with feathers
That perches in the soul,
And sings the tune without the words,
And never stops at all,
And sweetest in the gale is heard;
And sore must be the storm
That could abash the little bird
That kept so many warm.
I’ve heard it in the chillest land,
And on the strangest sea;
Yet, never, in extremity,
It asked a crumb of me.
Host:
Hope is the thing with feathers
That perches in the soul,
And sings the tune without the words,
And never stops at all,
How beautiful are those words? And hope is such a central theme in relational safety

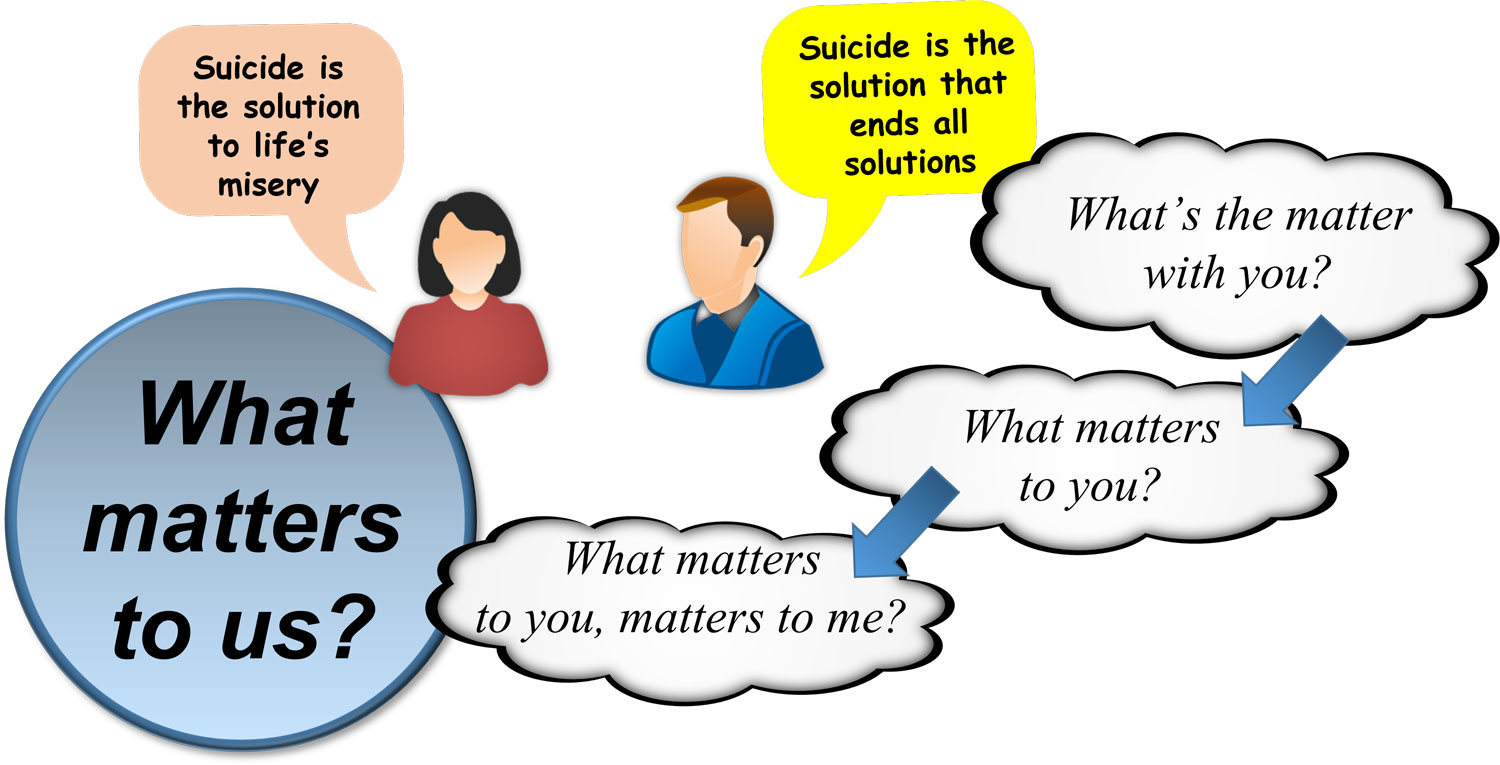
Expert: Yes, it is. In the first episode we discuss how suicide becomes the salient solution to the entrapment of life, a life of pain and hope is crucial in helping the person see that there is a way out that does not entail ending one’s life.
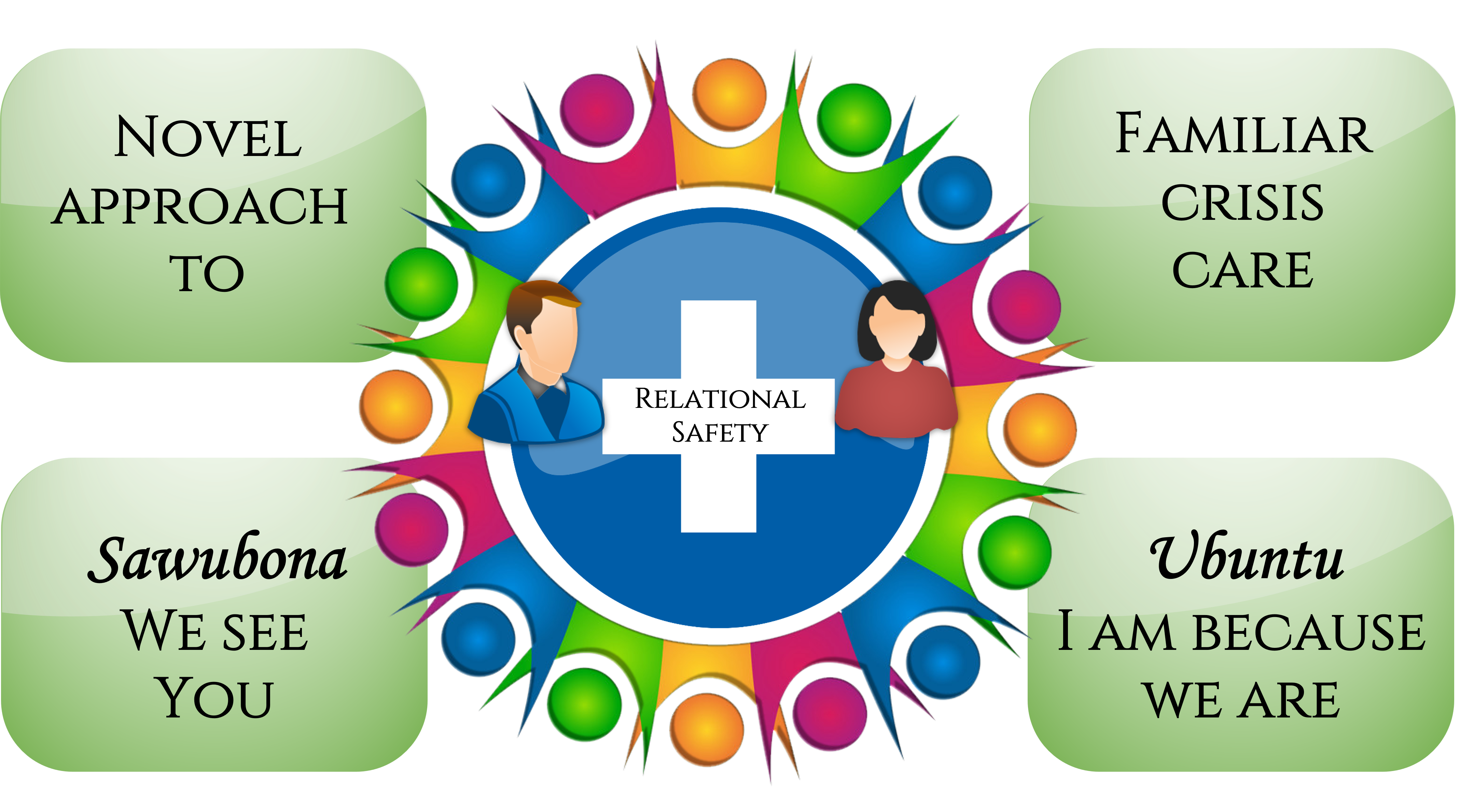
Host: You talk about how hope comes out of an empathic connection, connecting with a person and creating relational safety. You use two Zulu words to capture the essence of relational safety.
Expert: yes the first is Sawubona, it’s a greeting, a hello meaning we see you, me and my ancestors see you, not just you, but you and your ancestors, your hopes, your dreams, your aspirations and in the process of seeing we bring you into being. To create relational safety for a person in suicidal distress, perhaps that is the way in which we need to see and listen to the person. The relationship itself becomes the springboard for recovery. This is captured in the second word, Ubuntu, I am because we are, recovery is a journey of hope that is done together, in partnership. This is the golden thread that runs through PROTECT, how to use the healing power of human relationship, how do we make a person in suicidal distress experience truly experience Ubuntu.
Host: You then go on to talk about the origins of PROTECT lying in the work that you did in the national award winning PROMISE project and the internationally acclaimed 3-3-3 system of acute care in Cambridge
Expert: yes, and I think I end with the metaphor of these podcasts being similar to the act of purchasing new clothes for an existing wardrobe. It does not mean that the old wardrobe has to be discarded as a new suit might go very well with a shirt and tie from what already exists. The knowledge and skills from PROTECT will complement those that already exist in an experienced clinician and for beginners in mental health it will provide a solid foundation.
Host: So that was episode 1, episode 2 was the nautical metaphor of Navigating Rocky Waters
Expert: To help our colleagues draw inspiration from individual recovery journeys of our patients we used a nautical metaphor. There is a fundamental contradiction at the heart of mental health services between care and control. This is particularly the case when supporting someone in suicidal distress. Worldwide mental health services have been guided by the recovery philosophy on their transformation journey. Capturing hope, creating agency and realizing a life beyond illness underlie all that we do. We are acutely aware that there is no place for force in recovery. However, the use of force continues, we believe that proactive systems of care can help us navigate through the choppy waters of the care and control contradiction. PROTECT stands for PROactive deTECTtion. A theme that will emerge as we go through the podcasts of ASSESS and ASPIRE is that is it possible to make the use of force and restrictive practices redundant through proactive systems for detection and prevention. Navigating Rocky Waters was written to portray how seemingly binary positions like risk and recovery or care and control are part of a spectrum, without risk there is no recovery, with the right care the person in distress does have more control. Episode 2 is full of life jackets, lifeboats, anchors, lighthouses, maps, compasses, etc.
Host: Episode 3 builds on this metaphor of being at sea and introduces the Care Compass
Expert: Yes we use an accentuated version of navigating rocky waters to capture how delicate is the balancing act between risk and recovery and how using the care compass one may fine tune control in care.
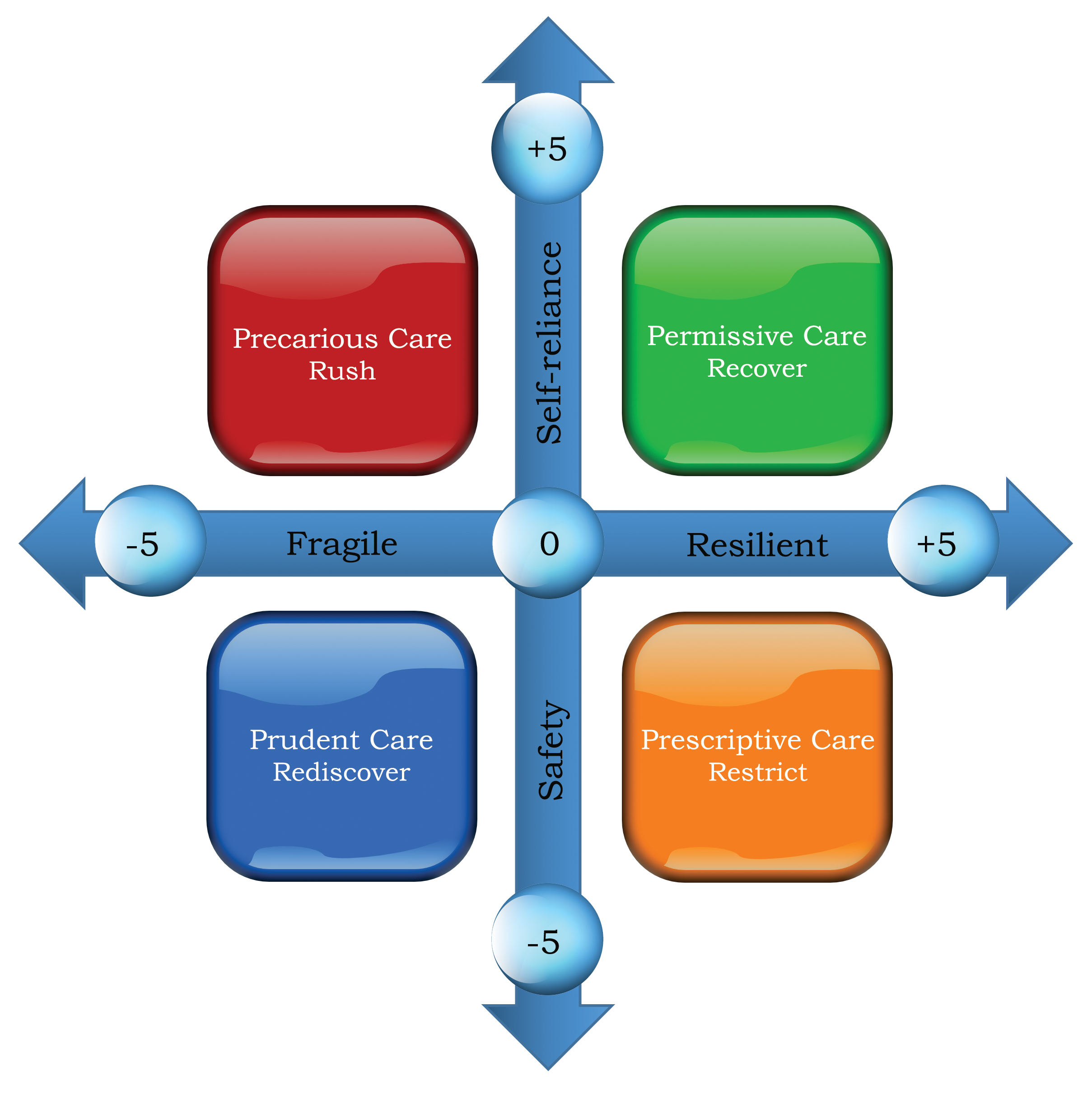
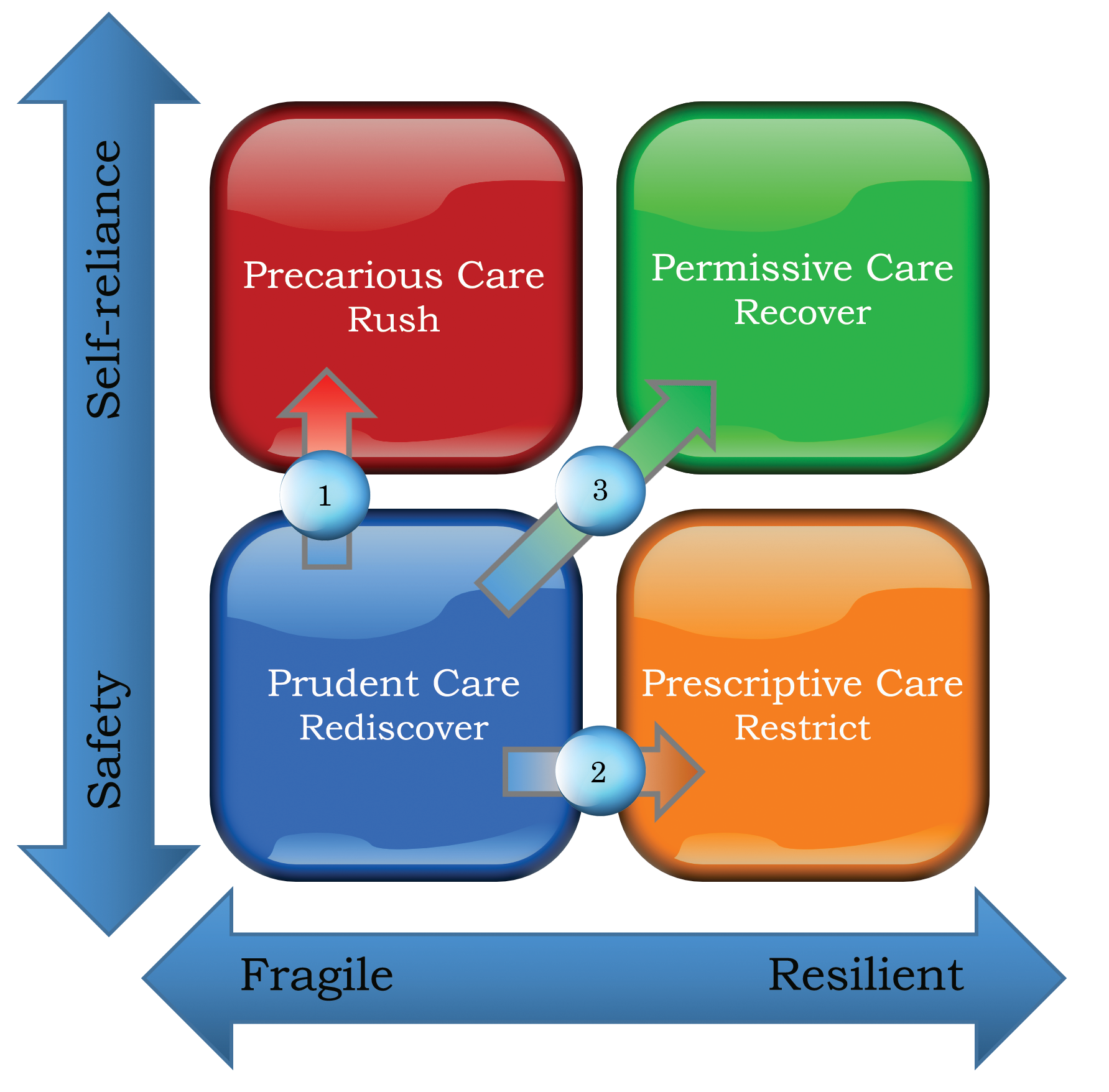
Host: Can you remind our listeners about the four quadrants of the Care Compass
Expert: Sure, the Care Compass has two axes: x represents resilience in the distressed individual (East or the right end of the axis: resilient; +5 and West or the left end: fragile; -5), and y represents the principal focus of care delivery for the professional (North or the top end: self-reliance; +5 and South or the bottom end: safety: -5). The numbers + or – 5 does not indicate right or wrong, it is just to graphically demonstrate the degree of resilience in the person on the x axis and the clinician’s primary focus on the y axis. The two axes gives rise to four care quadrants, bottom left or south west: Prudent Care, the key word being rediscover, people are at their most fragile, and the principal clinical focus is safety, top right or north east: Permissive Care, People feel resilient, and the focus shifts from safely navigating the crisis to becoming self-reliant, the key word being recover, bottom right or south east: Prescriptive care, people are feeling resilient too, but the focus of care has remained on safety, the key word being restrict and top left or North West: Precarious Care, people are still quite fragile, but instead of focusing on safety, the clinical priorities have shifted prematurely to gaining self-reliance, the key word being rush.
Host: In the fourth episode you flesh out the Care Compass further and provide pragmatic ways in which it can be used to conceptualise and understand recovery and the various pitfalls in the context of suicidal distress, you talk about how to use the theoretical framework in delivering clinical care, to capture hope, to provide an understanding of risk and safety, to resolve differences in opinion with the person and their family.
Expert: approaches to risk vary quite considerably, when we encounter someone in suicidal distress to begin with most professionals will operate in the prudent care quadrant, under ideal circumstances the hope is that the person will become more resilient and the clinical focus will shift from safety to self reliance, so a move from the bottom left prudent care to the top right permissive care where services can take a step back, in order to make that happen measured but positive risks have to be taken, however some professionals and organisations are quite risk averse and care moves across to Prescriptive care, there are also situations where due to resource constraints or risk prone decision making, care moves into precarious care. Having this diagrammatic representation of positive risk taking, risk averse and risk prone practice helps significantly with reflective practice, helps in engaging the person and the family in conversation about where we are now, where we are headed and how will we get there. This way once can capture hope, provide better understanding of what recovery will entail and also resolve differences in opinion.
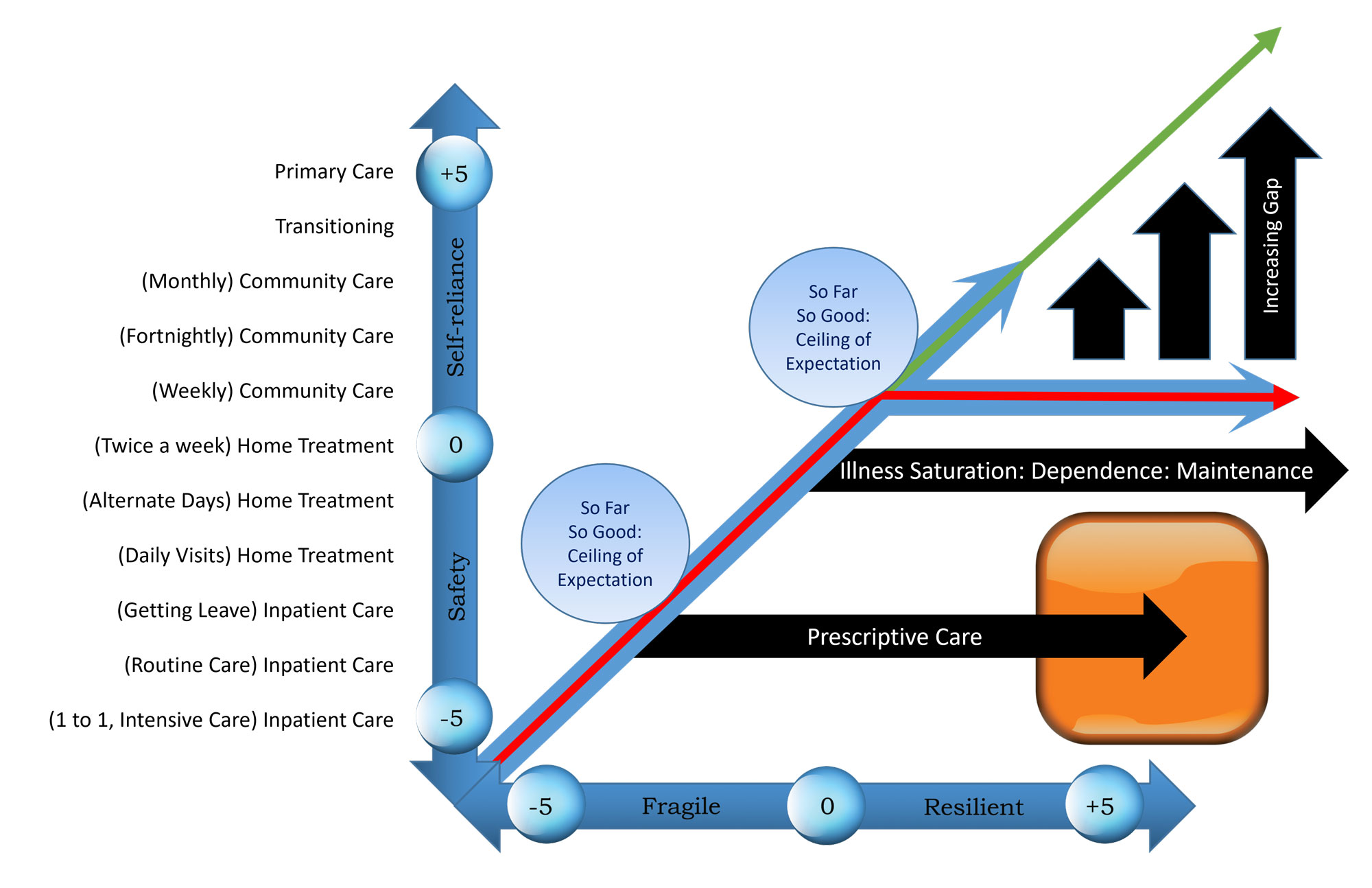
Host: As always please do look at the PROTECT Guidebook or on the podcast blog www.progress.guide/blog for the figures and images, it is so much easier to understand what Manaan is talking about if you have the images in front of you. You then go on to talk about illness saturation due to maintenance treatment.
Expert: I think this is the most complicated diagram in PROTECT, works well on a video with the multiple arrows but really difficult to talk about in a podcast without the image so your advice is well placed. Essentially there is the person’s projected trajectory from the bottom left to the top right, but somewhere on the way when professionals start reviewing people once a fortnight, they unknowingly set up a ceiling of expectation for the person, the person hits the ceiling and begins to track along with the professional, beginning to believe that in order to stay well they need fortnightly or monthly reviews. Thus there is an ever increasing gap with time between where the person should have been i.e. the professional would have no role in the person’s life and where they end up feeling dependent on ongoing professional support. This can happen on a ward with long stay patients, but because of pressure on beds people are mindful of value added by staying on a bed, but this is very common in the community. Reflective practice using the care compass can help mind the gap between what a person can be and what they might become if we do not let go in a timely fashion.
Host: Moving on to episode 5, optimise pain relief, this is a fairly popular episode with our listeners, care compass was all about striking a balance between risk and recovery, in Optimise Pain Relief you translate this balancing act into a delicate conversation about death and life by creating a narrative of pain and the desire for pain relief.
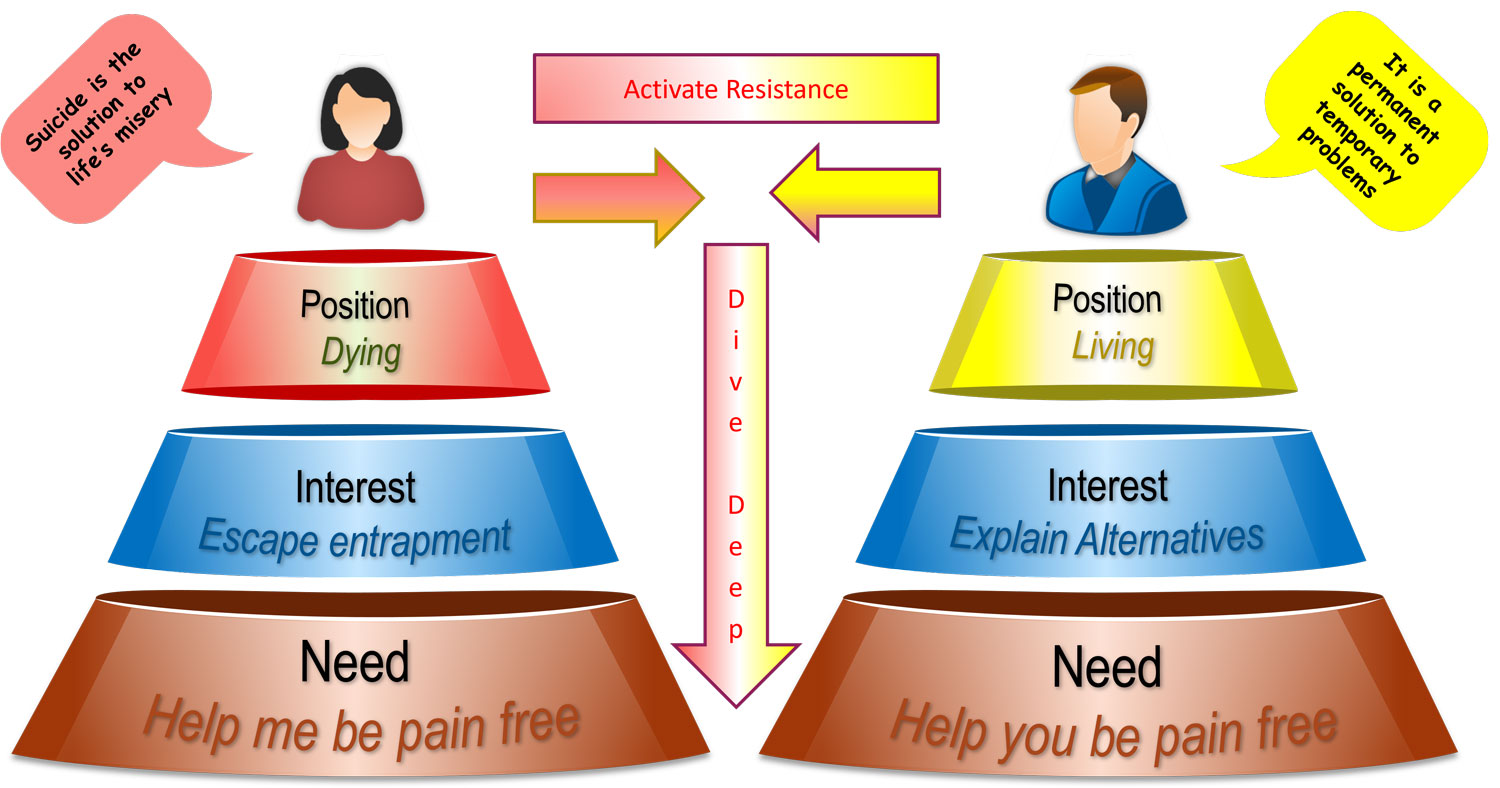
Expert: This narrative is the foundation of relational safety and avoids the power struggle that can so easily break out between the professional and the person. To gain an alternative perspective into the mind of a person in suicidal distress, we recommend an approach in which the professional dives deep to establish the interests and needs that underlie the position of dying. When faced with the ambivalence a person is experiencing towards life, professionals need to temporarily relinquish their strong desire to pull over the person from their death orientation to one of living. This requires courage as it might go against all that the professional believes in and is trained in. Gain an understanding of how the underlying interest to escape entrapment and the need to be pain-free manifests as suicidality. Construct a pain based narrative and help the person see that their desire to eliminate excruciating pain is a justifiable response, a response they share with all other living beings. This validation will go a long way in establishing the safety partnership. But above all, seek first to understand and then to be understood. Explicitly articulating to the person why a pain guided desperate measure seems like a reasonable response is healing in its own right. Professionals want to help a person in pain be pain-free. So they begin to explain alternatives to suicide prematurely. The challenge of empathy demands that professionals do not focus on “what they need to say” but “what the other needs to hear”. What a mind in crisis needs to hear is an empathic acceptance, that their suicidal desire, their thoughts and actions are undertaken in the interest of escaping entrapment and the need to be pain-free. The professional must comprehend this connection first. If they do, not only can they understand the apprehension to the offer of help in terms of life and living (i.e. safety) as it equates to more pain, they can then guide the person to see how in their desire to eliminate the pain they are eliminating life. In terms of pain relief, the alternatives may be much slower than suicide, but there are effective ways of either chipping away at the pain or improving one’s tolerance to it. When a professional can explain these connections with openness and honesty, not only do they gain the trust of the individual but also the commitment to work together towards a life orientation that does not involve a power struggle, there in constructing relational safety.
Host: In episode 6 we moved on to Risk Rethink, from memory the first point you made was how a simple risk factor driven approach to risk assessment and prediction does not work.
Expert: Yes that’s correct, even the strongest risk factor like 90% of people who take their lives through suicide have a diagnosis of a mental illness (Jobes 2006) are not much use. In secondary mental health care, every patient has a diagnosis. This makes the presence or absence of the same redundant as a predictive risk factor. The same can be said of most risk factors when considered independently, e.g. of the millions who are socially isolated, very few go on to suicide. It is the interaction between different risk factors which takes a person from ideation to action, the factors on their own do not help us differentiate who is just thinking about it from who might act.
Host: So you recommend focusing on warning signs.
Expert: All warning signs are risk factors but not vice versa, the key difference being time. Warning signs are dynamic, temporary and capture an acute escalation of risk rather than static suicide risk in the longer term. Attempt to arrive at opinion on clear and imminent risk, the next day, the next week, the next fortnight, cause that is where you can make a difference, beyond that there are way too many factors to take into account.
Host: You then described the cubic model
Expert: Yes Shneidman’s cubic model introduces the listeners to a continuum of risk rather than static categories. Risk can move along the three axes of the cube, psychache, stress and perturbation, so at one end is 000 – no risk and the diametrically opposite end is 555 – that corner cubelet is the diagrammatic representation of clear and imminent risk. In between the two corners are 123 other cubelets within which risk fluctuates based on what is going on in the person’s life.
Host: And you gave simple examples of risk management in terms of how someone who is at a 555 could be moved to a 4 on any of the 3 axes and that might avoid someone transitioning from ideation to action.
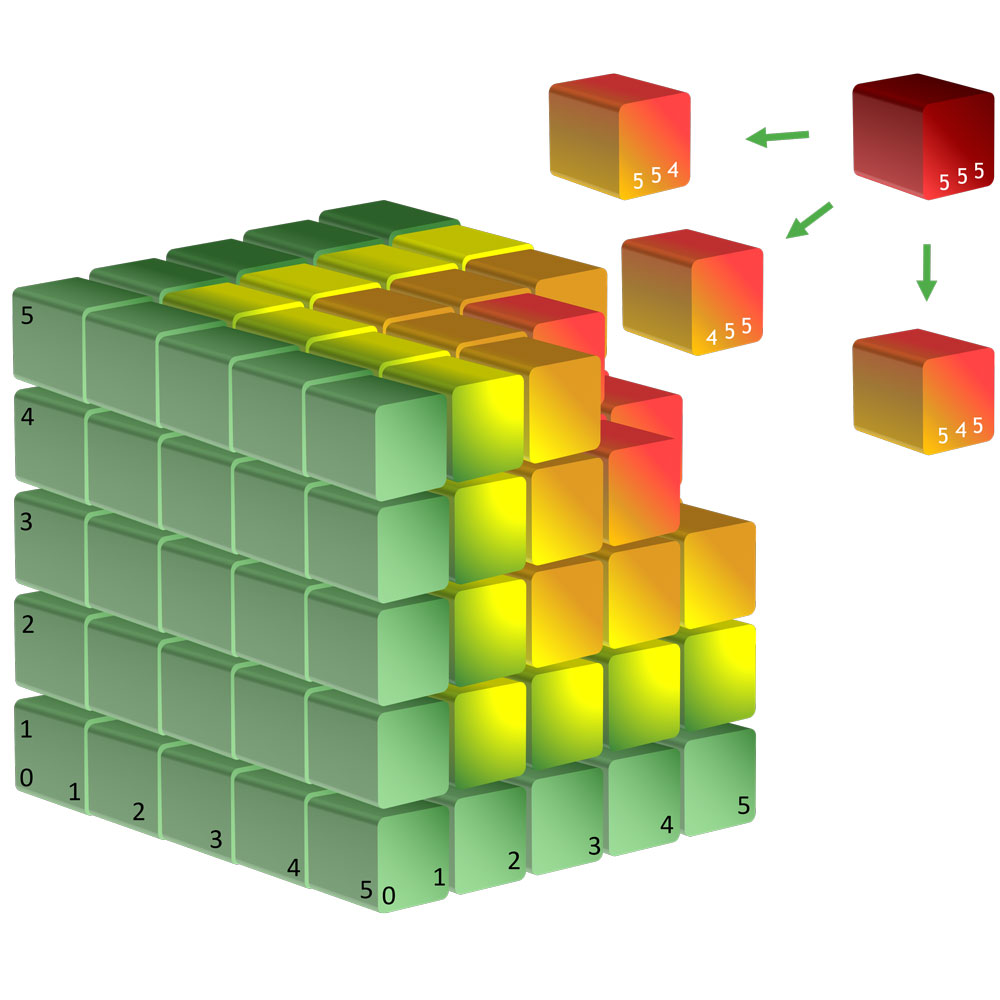
Expert: Yes and a 5 to 4 may be a simple conversation like the ones that take place during an assessment in which hope is captured or the promise of medication that might work or therapy that may help, sometimes that is all that is needed, of course suicide prevention is much more complex than this, but I love the simplicity of Shneidman’s cubic model and how it makes us think of risk in three dimensions rather than a one dimensional linear approach.
Host: In episode 7 you build on the concept of a continuum further and site the overwhelming evidence for the futility of risk categories of high, medium and low.
Expert: And the evidence comes from a number of sources, large metaanalyses which show that our predictions are quite poor in terms of outcomes, the national confidential inquiry shows that 83% of females and 86% of males who suicided within 7 days of contact with services had their short term risk rated as low or none. A finding that is corroborated in our own data, so why engage in a clinical activity that is fundamentally flawed.
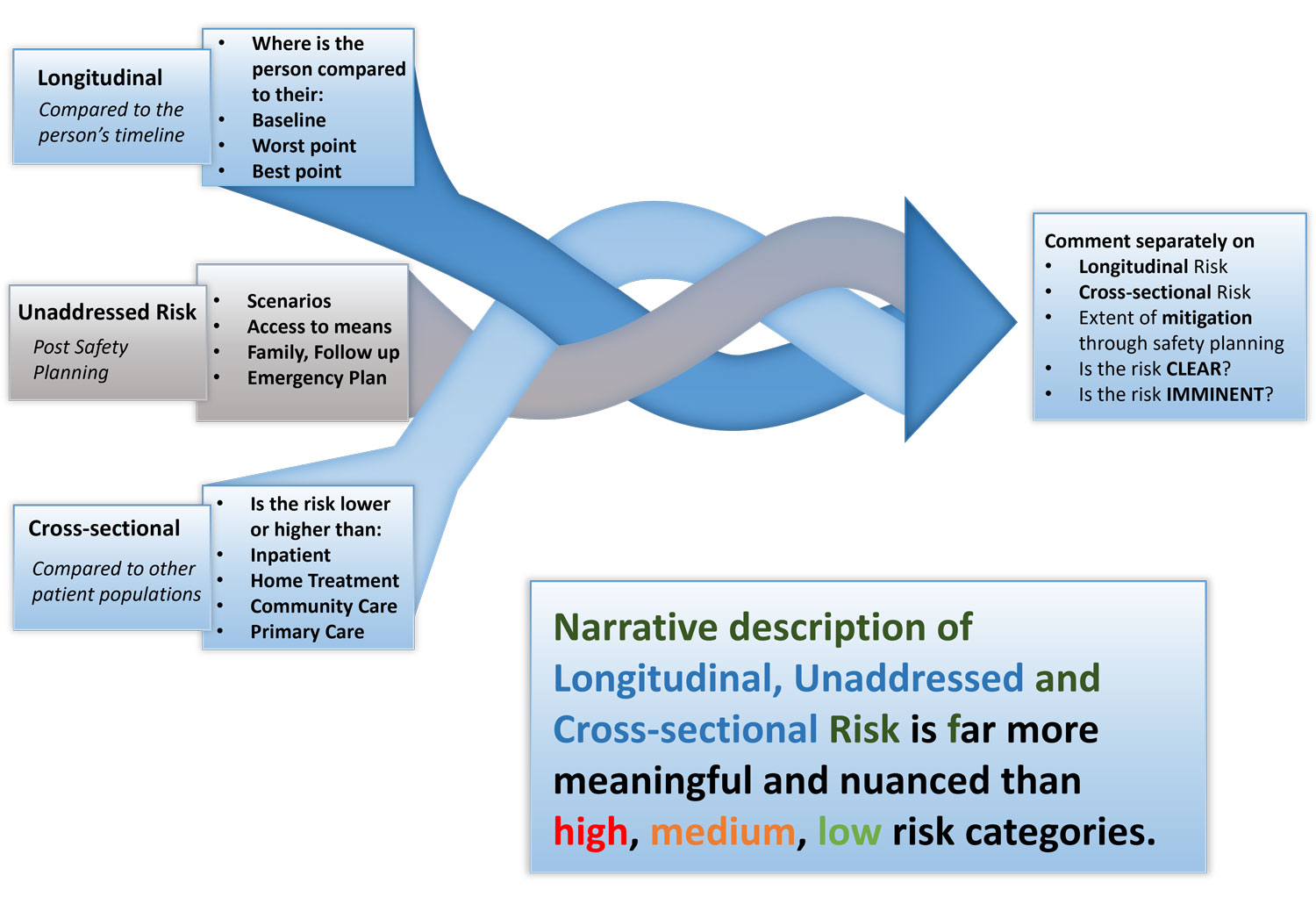
Host: And you provided an alternative to high, medium and low using longitudinal risk, unaddressed risk and cross sectional risk as a way of arriving at an opinion on clear and imminent risk.
Expert: Yes, this is a unique and novel way of formulating risk, longitudinal risk is the person’s risk over time, how it fluctuates in relation to their baseline or worst point, is it getting better or worse, unaddressed risk is risk that is left unmitigated post safety planning and cross sectional risk is the risk compared to different populations, it involves mindfully pausing and asking oneself at this point in time is the risk similar to those who are inpatients or community patients in secondary care or are they similar to those in GP land. The different perspectives when intertwined provides a clear picture of whether the risk is clear and or imminent and the opinion can then guide the professional towards the next steps in terms of what treatment is needed and where it is best delivered and by whom.
Host: In Episode 8 you talk about Roger Bannister and Mindset shifts.
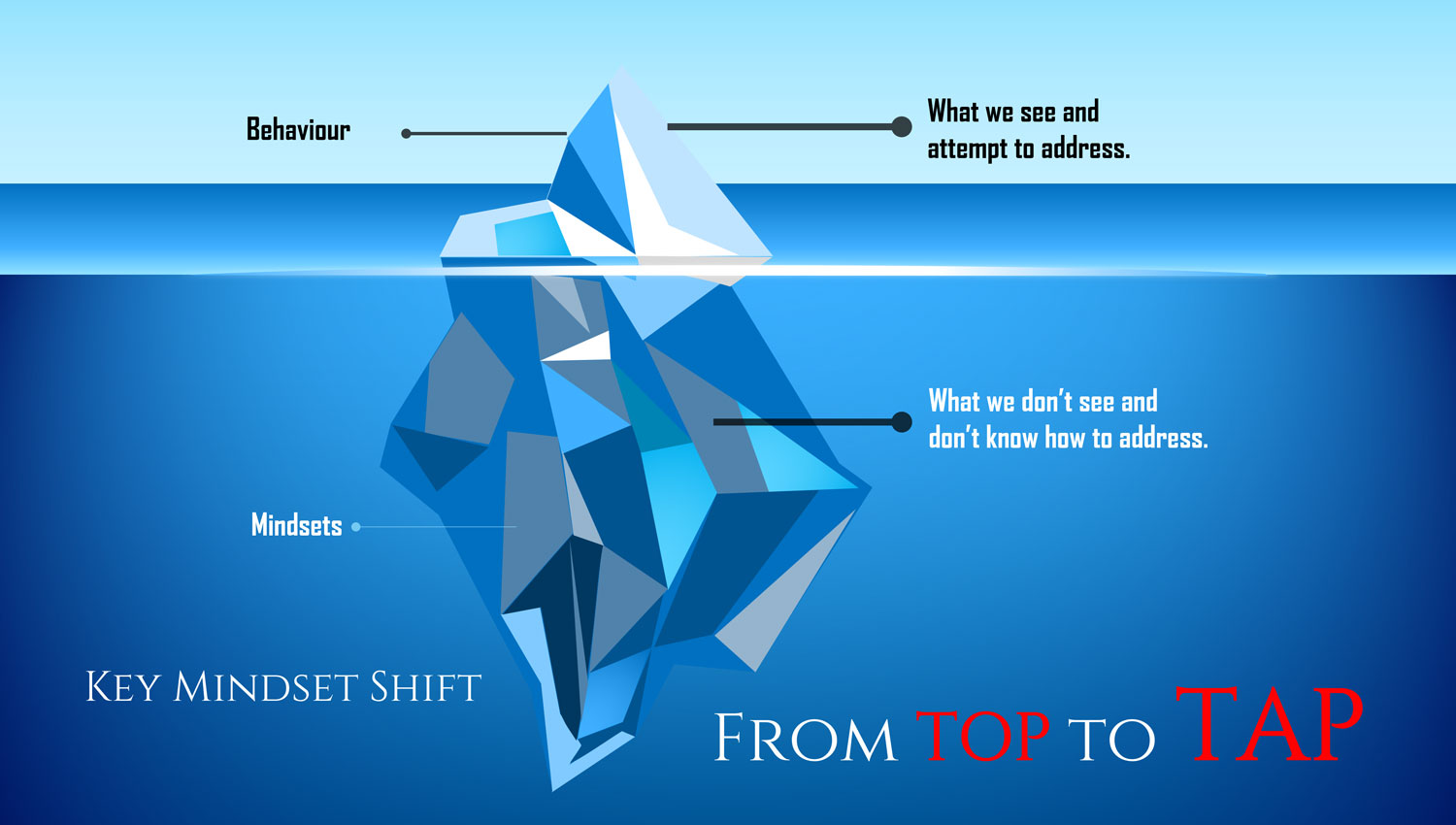
Expert: If you don’t mind I would like to hold on to the discussion of the mindset shift from top to TAP for the beginning of the next episode as I want to link the mindset shift to three practice changes that lie at the foundation of the ASSESS and ASPIRE module. Also we are in the production phase of a new course called 7 SAFE Steps for safety planning and risk management on inpatient wards, something that I am really excited about and the mindset shift and practice changes are a crucial part of care delivery, so I would like to begin the next episode with the mindset shift and the practice changes that result from it rather than late into a podcast.
Host: Of course, in episode 8 you also talked about how COVID impacted professionals and people with mental health challenges in the same way, people are on different boats but in the same storm.
Expert: Yes COVID created a commonality of experience, it has shown us that irrespective of role, what matters to you matters to me too. So why should anyone be on top when the narrative of what matters to us demands that we are on tap. But we will talk about top to TAP shift in a bit more detail at the beginning of the next episode.
Host: In episode 9 you introduced the values of relational safety.
Expert: the 5 Core values:
- Courage: to be present and suspend the desire to help
- Curiosity: in taking the time to listen and recognizing reasons and emotions
- Compassion: in sharing the person’s darkness without judgement
- Commitment: to reframe suicidal thoughts and acts as a desire to be pain-free
- Collaboration: to coproduce the journey ahead based on mutual respect
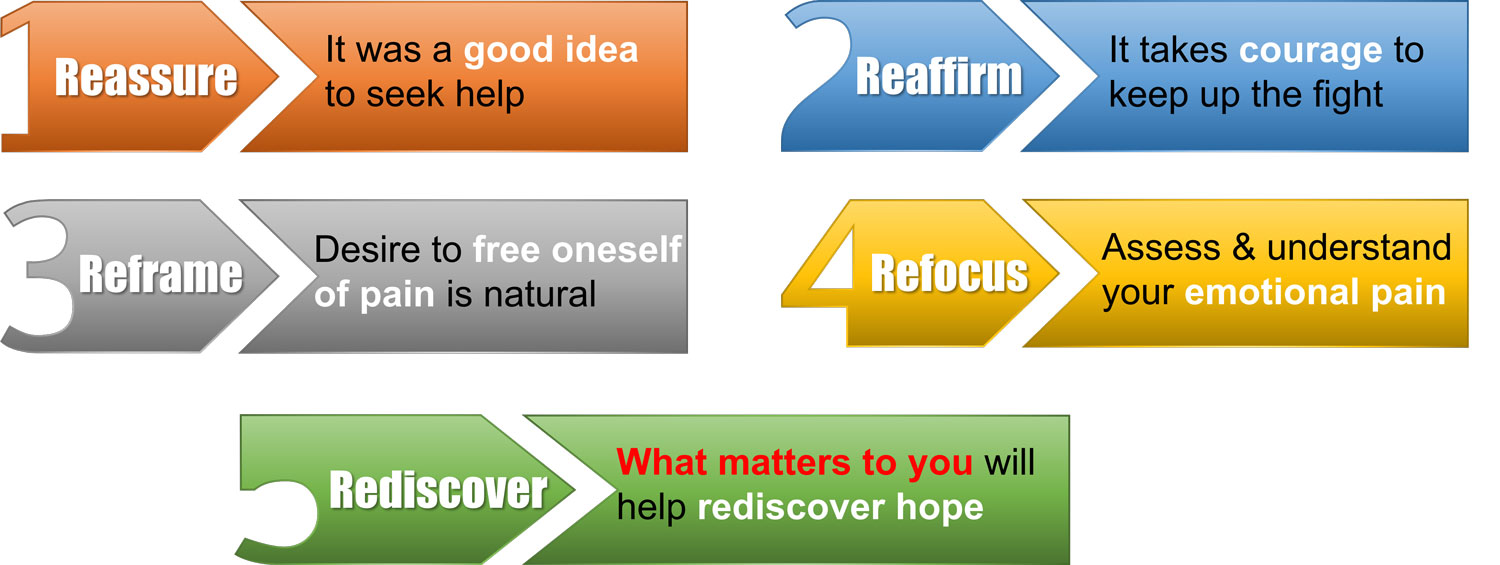
Host: and then you brought it together into the pain relief dialogue with the 5 actions: Reassure it was a Good idea to seek help, Reaffirm their Profound pain, Reframe it as an Understandable response, Refocus the Assessment as one of pain, Rediscover What matters
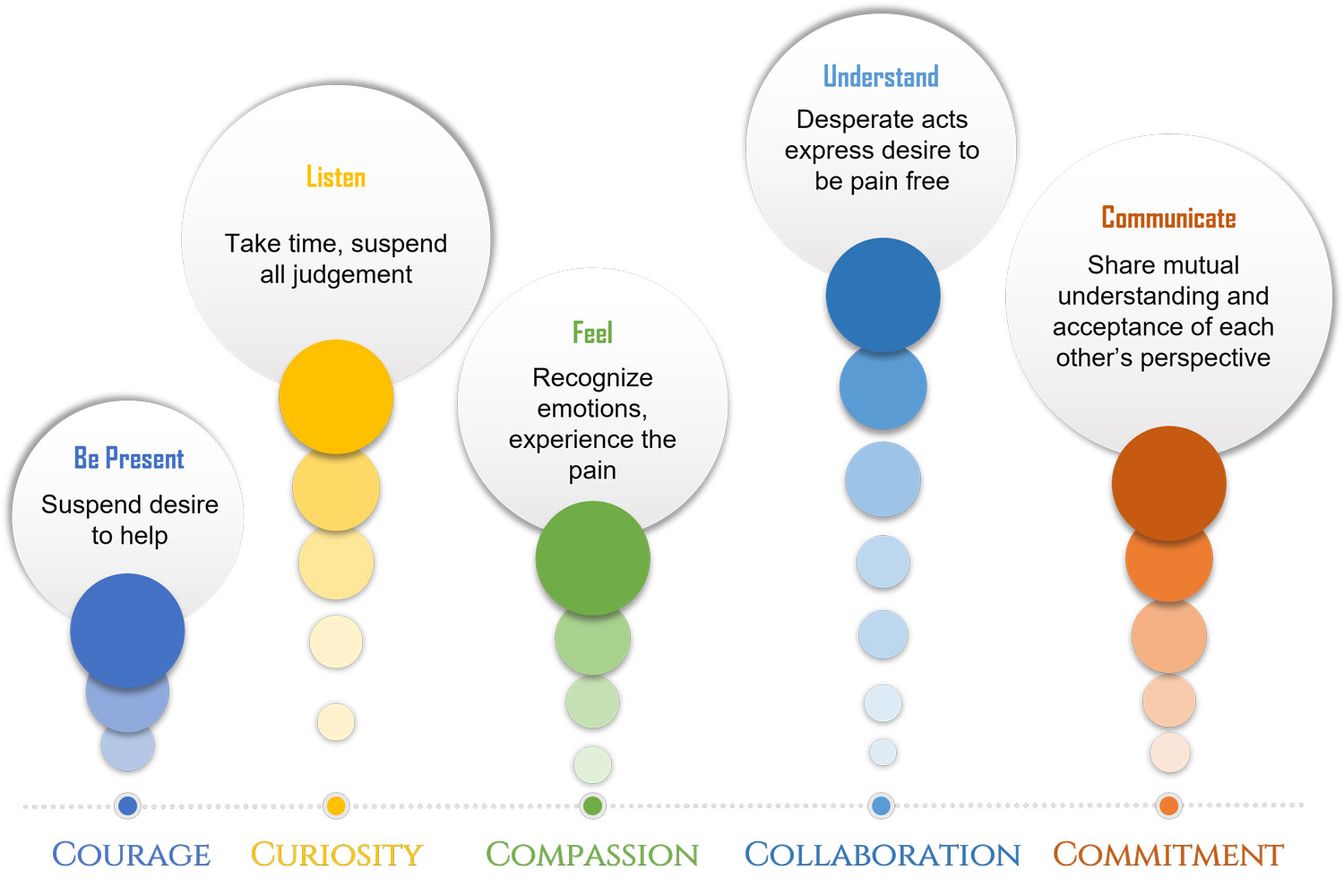
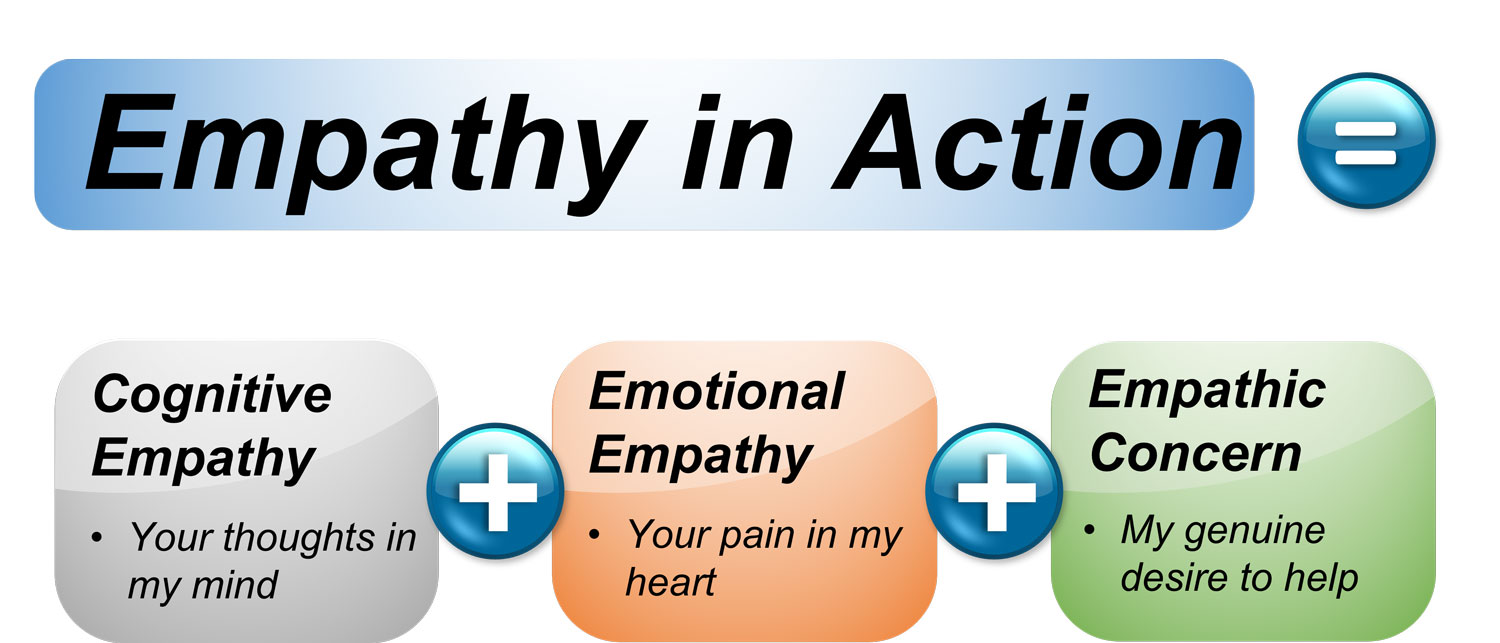
Expert: The pain relief conversation takes less that a minute, but it is invaluable in terms of forming rapport and creating relational safety, once you have said those words, essentially you can ask anything as you are attempting to get to the bottom of the pain, so that you can chip away at it. It comes across as your genuine desire to help. Living the values constructs empathy in action. To remind our listeners, there are 3 specific components, cognitive empathy – I think I have gained a sense of how you are thinking – your thoughts in my mind; emotional empathy – I feel what you are going through – your pain in my heart and, finally, empathic concern – the genuine desire to help someone in their hour of distress.
Host: and finally in episode 10 you translate the values into action, when one lives the values in an interaction, how does the interaction look like.
Expert: For each of the values we make points about practical application of the values, lets just quickly run through them. Regarding the Courage to be present we talk about how difficult it is to suspend the desire to help, how our mind keeps wandering towards solutions, instead we recommend living the value of curiosity and listening with fascination, mind open, mouth shut, so suspend all judgement and listen with complete attention, show Compassion, get up close and personal, close enough to feel the pain but not so close that you get overwhelmed and cant think straight, be aware of compassion fatigue, one cannot pour from an empty cup, collaborate with the person, listen to understand and not just to respond and Commit to your promise of recovery and walking by their side, believe that with the right support things will get better and soon. The 5 values together bring to life empathy in action.
Host: Yes, last week had all the catch phrases, I remember patient is not in the way, patient is the way, listen with fascination, mind open – mouth shut, cant walk through water without getting wet, an explicit promise of recovery, things will get better and soon. Did you take the time to tweet what was your favourite? Tweet it at #GuidePorgress. It helps get the word out about the podcast to more professionals. This brings us to the end of episode 11, hope it will serve as a refresher for the CORE module. In the next episode, we will introduce the different chapters of the ASSESS module but before that we would go over the key mindset shift top to TAP and the 3 practice changes that Manaan is being very mysterious about. You can access all the information at www.progress.guide. We would love to hear your thoughts, you can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide, you can email us at admin@progress.guide. We are also on twitter and youtube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on spotify, apple podcasts or audible or whichever channel you are listening on. Providing healthcare professionals contemporary knowledge about how to connect and create relational safety is crucial in suicide prevention. Remember together we can make a difference. Tune in next Friday and we will share with you a bit about the new program called 7 SAFE Steps for inpatient psychiatric care. Thank you for joining us today and keep spreading the word.
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience