08 | Empathy in Action I – Top to TAP
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date February 25, 2022
Host: Good day, I am Mahi, your host for episode 8, we have made it to the final chapter in the CORE module, Empathy in Action. For the last two episodes we kept saying that we will dive into a discussion regarding mindsets but we keep running out of time. Well today is the day, but first a quick recap. So far we have completed three chapters from the CORE module. The first, Care Compass focused on the balancing act that professionals need to strike between risk and recovery, the second, Optimise Pain Relief provided strategies for creating a pain based narrative on the road to discovering common ground. And in the third, Rethink Risk we explained the futility of risk stratification, guiding listeners from a categorical approach to one in which risk is a continuum. Manaan, will you please provide a summary of how professionals should formulate risk?
Expert: Within the PROTECT training we strongly recommend that clinicians should use warning signs to opine on clear and imminent risk, cause that is where they can have a meaningful impact. Opinions about longer term risk are academic in nature, way too many factors that are beyond the influence of the clinician and the person at this point in time.
Host: And you mentioned longitudinal risk, unaddressed risk and cross sectional risk as a way of arriving at an opinion on clear and imminent risk.
Expert: Yes, this is a unique and novel way of formulating risk, longitudinal risk is the person’s risk over time, how it fluctuates in relation to their baseline or worst point, is it getting better or worse, unaddressed risk is risk that is left unmitigated post safety planning and cross sectional risk is the risk compared to different populations, it involves mindfully pausing and asking oneself at this point in time is the risk similar to those who are inpatients or community patients in secondary or are in GP land.
Host: This way the opinion can then guide the professional towards the next steps in terms of what treatment is needed and where it is best delivered and by whom. Remember to access the diagrams from www.progress.guide/blog or get the PROTECT Guidebook from Amazon to read along while listening to the podcast. There are also video courses at www.progress.guide/courses. Let’s get on with today’s show, Mindsets. What is a mindset and why are you obsessed with them?
Expert: Have you heard of Sir Roger Bannister?
Host: Of course, the one who broke the four minute mile.
Expert: Yes, but there is a bit of history and legend to this. On May 6, 1954, the announcer at the Oxford University cinder track in England calmly gave the placings in the one mile race, and then started to announce the winning time, beginning with the word “three…” The small crowd erupted in delirious excitement, the rest of the announcement went unheard, and Roger Bannister became an instant legend as the first man to run the one mile faster than four minutes. His 3:59.4 that evening is often cited as one of the seminal moments in the world of sports. It has become a symbol of human achievement on the same level as the conquest of Mount Everest the previous year (May 29, 1953).
The First Four Minute Mile - #BeInspired
Host: Ok, amazing achievement, but what has that got to do with mindsets
Expert: This is not just about Bannister. Before he smashed the 4 minutes, it was a scientifically established myth that this was humanly impossible, and he did it on a wet, windy day in Oxford. Achieving the impossible was an amazing feat. However, within two months, John Landy from Australia ran the mile below four minutes, and over the next three years, 16 other athletes completed the same feat. Yet until 1954, this was considered beyond human reach. What happened? These were not mutants running the four-minute mile; Bannister broke through a glass ceiling, showing it can be done, bringing about a shift in the mindset of all athletes to follow.
Host: I think I get what you are getting at, Bannister uncapped dormant human potential that no one knew existed. But how is the four-minute mile relevant to suicide prevention?
Expert: I am using the four minute mile to show how results and outcomes can change, when the lens through which we are viewing the scenario and in our case the person in suicidal distress changes. You see the world had talked of sub-four since the heady days when the “Mile of the Century” races in the 1930s enraptured huge crowds. During the war years, Gundar Haegg kept the sub-four passion alive, leaving the mile record at 4 minutes 1.4 seconds, but after 1945 no one had even come close to threatening the 4 minutes but once Bannister shifted the mindset to “it can be done” a whole host of expectations and behaviours changed in the running world and the new records came thick and fast.
Host: If I am following you correctly you are linking expectations that athletes had of themselves to the expectations professionals have of the interaction with the person in distress. And the athletes’ behaviour of how hard they will push themselves in training and on race day to the daily clinical practice of professionals.
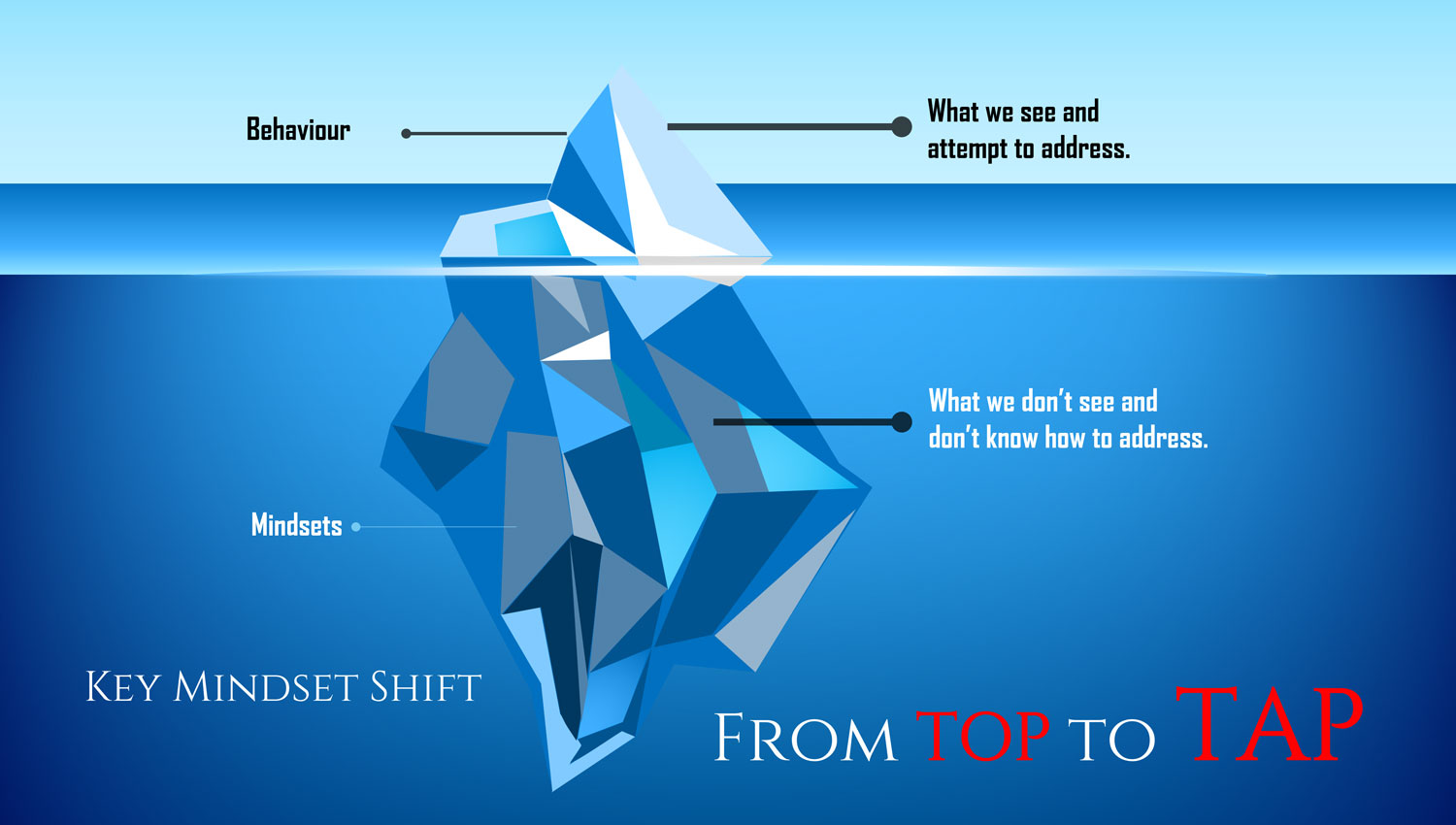
Expert: Exactly, clinical practice is akin to an iceberg. Only 3/10th is above the water; this is what we see and address. But the invisible 7/10th, the sum total of our beliefs, values, needs, both met and unmet, has a significant impact on how we behave and interact with a person in suicidal distress. These are the paradigms through which we make sense of the world – in other words, a mindset. Our mindsets dictate how we behave in the clinical sphere and how we deliver care.
Host: You are saying shifting mindsets is critical to practice change.
Expert: Yes, have you ever played whack a mole at an arcade.
Host: I haven’t, but I know what you are talking about, you hit a mole on the head with a hammer and another one pops up.
Expert: that’s right and you keep hitting these moles as they pop, attempting to change clinical practice without addressing underlying mindsets can feel a bit like playing whack a mole. Behaviour chasing is tiring and just does not work, but you change a mindset and a whole host of behaviours change automatically.
Host: Each chapter in the CORE module highlighted a delicate balancing act, risk vs recovery for care compass, the narrative of death vs life for optimise pain relief, category vs continuum for rethink risk and for empathy in action it is form vs function. I am assuming the desired behaviours relate to the functions of the forms like risk screens, that are filled in during an assessment.
Expert: Conventional suicide prevention courses attempt to improve clinical practice through different screens and tools. These are the forms that are filled in. They are meant to standardize the assessment process and add rigour to it, but their primary function is to guide a conversation, a conversation that is the foundation of relational safety, a scaffolding of safety within which the person can reconnect with hope and their own potential. If the professional forgets the primary purpose of the form, the forms soon degenerate into a tick box, pencil whipping form-filling exercise. Form must follow function, a conversation that creates relational safety. There is paperwork for proper work and this particular chapter Empathy in Action is about getting people to understand the true value of those forms in a guided conversation.

Host: To remind our listeners and if you haven’t listened to episode 1 or the earlier episodes, Relational Safety arises within a deeply empathic therapeutic alliance based on mutual respect, genuine curiosity, and a true acknowledgement of the overwhelming emotional suffering. Back to mindsets, how do we get to these mindsets? Surely, we must know what they are before we can begin to address them.
Expert: Pause, think and a deep dive of mindful questions, do you have any four-minute miles that are limiting your ability to fully realize the potential of the relationship that you are about to form with a person in suicidal distress? What are the mindsets that keep us entrenched within a deficits focus? What mindset shift will free us to realize the true potential of the person in distress and work in an asset-focused recovery-oriented way?
Host: In your experience when such questions are asked what insight is gained.
Expert: We believe that the key to unlocking the potential of the relationship involves a shift in the professional’s mindset of being the sole expert, the professional has to move from a position of power, where they are the source of knowledge and expertise, to one where they are partners in an enabling role, supporting the person to reconnect with hope and their strengths. The clinician brings professional expertise and the person in distress brings their unique lived experience.
Host: So, both have expertise and what happens when you combine them?
Expert: That’s when you get the magic of relational safety. To break through the four-minute mile of deficits oriented care and transform it into care that is assets focused, a mindset shift is urgently needed in which professionals move from TOP to TAP (Kar Ray et al. 2019, 2020).
Host: From Top to Tap, that has got a nice ring to it.

Expert: And when professionals make that transition they find themselves in a unique position to connect with the gift of hope and engage the person in a journey of recovery supported by a novel discourse of discovery that attempts to conceptualise the psychological pain in terms of what is important to the person. The thing is a deficits mind set is attempting to establish “What’s the matter with you?” An assets mindset attempts to establish “What matters to you?”
Host: In terms of practice change what does the mindset shift from top to tap look like, let’s say in the assessment process, if I were a patient what will be different for me.
Expert: So, the first change we recommend for professionals is to change what they are attempting to establish, that instead of attempting to establish “what’s the matter with you”, establish “what matters to you”. This will go a long way to help move from a deficits focus to an assets focus.
Host: and that is because a person will not get suicidal over things that do not matter to them.
Expert: What is important to them will lie at the heart of their psychological pain. If a professional can truly grapple with this, they will automatically understand what’s the matter with them, making the question redundant. However, if they begin with the things that are important, not only will their responses be empathic and effective, they will tap into the person’s strengths and begin to shape relational safety and recovery. This seemingly small shift is quite significant in the way we approach care delivery as it moves professionals from a deficits based model to one that is recovery-oriented and assets based.
Host: What kind of answers do you get when you ask what matters to you
Expert: Pause and Think: What are the things that matter to you and me? Food on the table, a roof over our head, kind, loving relationships, making a difference at work, contributing to society is a life that is meaningful to me. The reality is, what matters to you, matters to me too. People in suicidal distress are no different. Their pain often stems from those fundamental things which make life worth living. So the real question is, “what matters to us?”
Host: We all want the same things from life, that is a unique perspective to approach a person in suicidal distress.

Expert: the last 2 years, 2020, 2021 and even into 2022, living in a global pandemic has been a great eye opener. COVID has brought the similarity in vulnerabilities between staff and patients into sharp focus. The threat to health, life and livelihood during COVID-19 created a parallel pandemic of psychological distress to which hardly anyone has been immune. It showed us that the things that mattered to staff were the same things that mattered to patients, being in good health, being able to work, keeping their family safe and so on. The pandemic created a shared experience. Although in different boats, staff and patients were in the same storm. They made meaning together of a time that was uncertain and unprecedented. Human conversations with concern for each other irrespective of what role they had was seen everywhere. Reductions in staffing or the threat of staff teams having to go offline following exposure to COVID had forced every staff member to work in an assets focused fashion. They had to draw on the person’s strengths, capture hope and help them to be self reliant. Perhaps out of the adversity of the pandemic, there is a lesson or two regarding the professional’s role in the person’s life and the approach we generally take. COVID-19 showed us that patients or professionals, when it comes to what matters, we are the same, so let’s connect at a human level with genuine curiosity to establish the source of the pain.
Host: That is true indeed, COVID has shown us that irrespective of role, what matters to you matters to me too. So why should anyone be on top when the narrative of what matters to us demands that we are on tap. This brings us to the end of episode 8, part 1 of Empathy in Action. In the next episode we will dive deeper into the values that underlie Empathy in Action. You can access all the information at www.progress.guide. We would love to hear your thoughts, email us at admin@progress.guide. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Providing healthcare professionals contemporary knowledge about how the forms they fill can actually serve the real function for which they were designed is crucial in suicide prevention. Remember paperwork for proper work. The real function is to guide a conversation, a conversation that is at the heart of relational safety. This can be achieved by moving from top to tap. Don’t seek to establish what’s the matter with you, rather what matters to you. You can be a vector for spreading this knowledge at your work. Thank you for joining us today and keep translating empathy into tangible action.
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience