05 | Optimise Pain Relief
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date February 4, 2022
Optimise Pain Relief - Relational Safety: The Journey from Pain to Pain Relief
Host: Good day, I am Mahi, your host for episode 5, Optimise Pain Relief. This is the second chapter in the CORE module, the first, Care Compass was all about striking a balance between risk and recovery, the second, Optimise Pain Relief translates this balancing act into a delicate conversation about death and life by creating a narrative of pain and the desire for pain relief. This narrative is the foundation of relational safety. Manaan, will you please elaborate on relational safety and how does one go about creating it conversationally?
Expert: The safety created within the scaffolding of a deeply empathic humane response is what we refer to as relational safety (Kar Ray et al. 2020). Exploring the suicidal darkness of a person in deep distress begins with the acceptance that the light of hope may be met with scepticism and resistance. Acceptance of ambivalence towards life and living allows for an empathic response. The professional can then truly grapple with the individual origin and course of development of psychache (Shneidman 1993). The term coined by Schneidman seeks to capture the intense psychological pain of a mind trapped in suicidal distress. In the face of overwhelming life challenges, suicide becomes the salient solution to the problem of life and the associated unbearable pain emanating from it. Effectively, thoughts, plans or acts of suicide become a proxy for pain relief or its promise (Kar Ray et al. 2020).
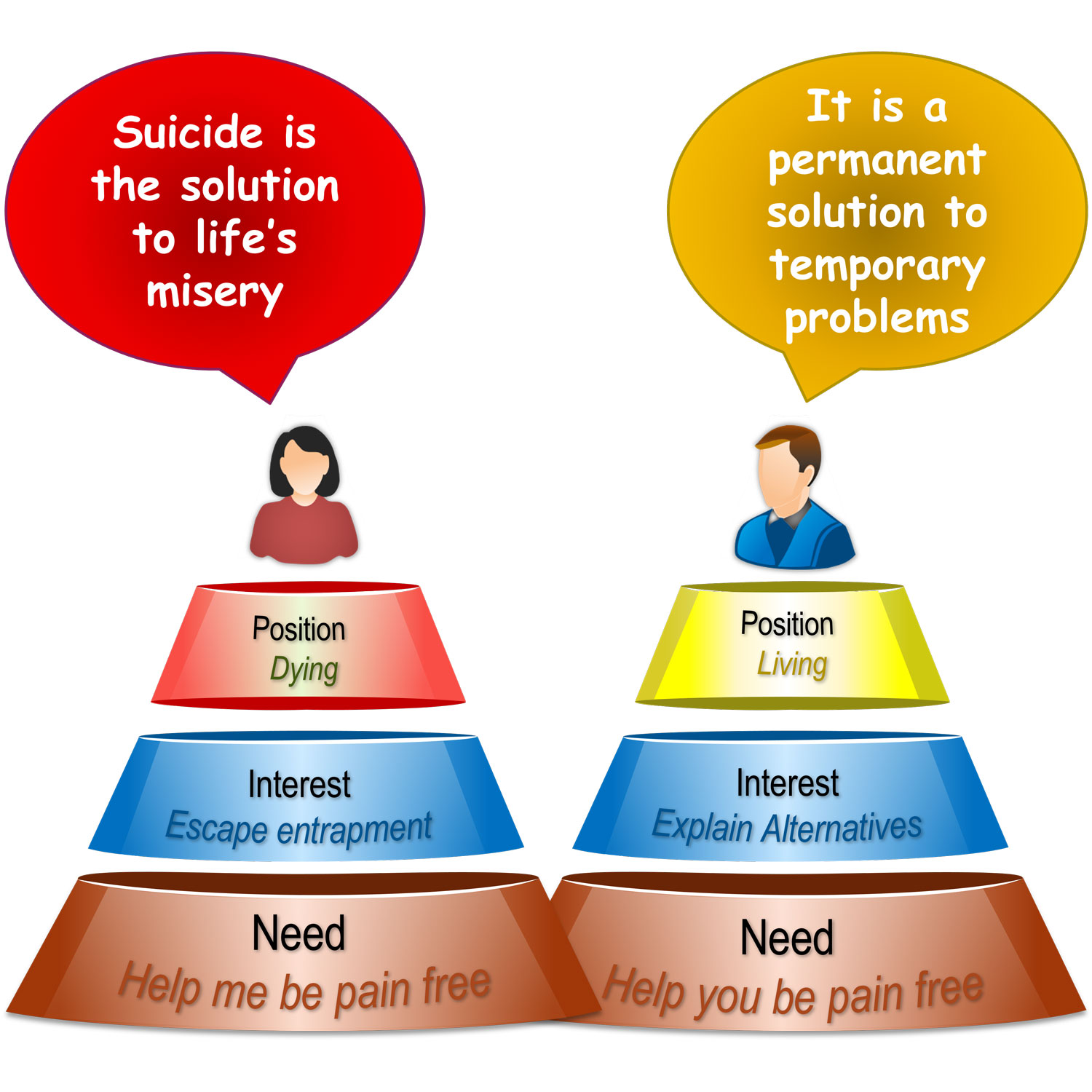
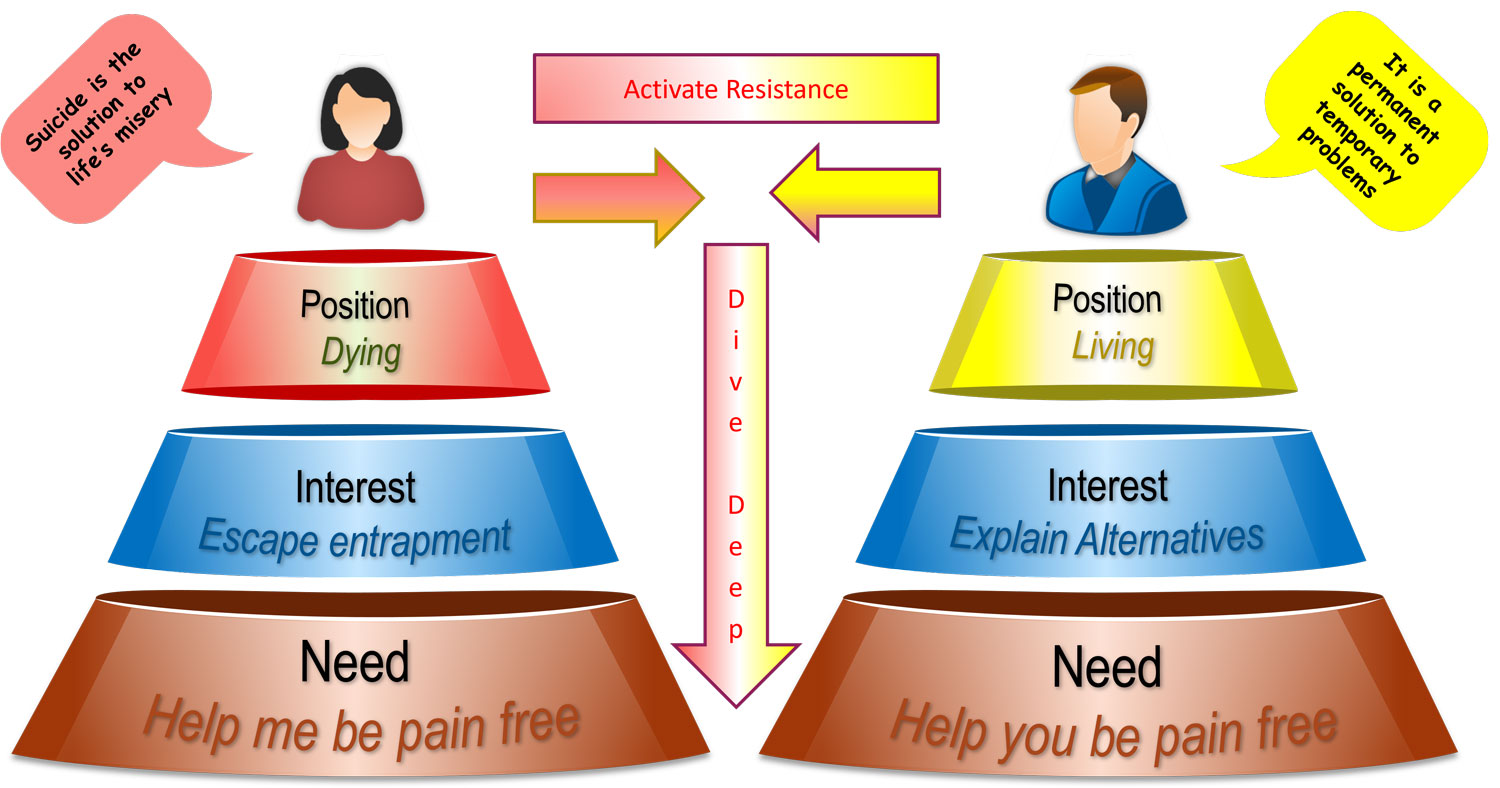
Host: You are saying that pain or the desire for pain relief is at the heart of the dissonant positions of dying taken up by the person needing support and living taken up by the professional supporting. The person considers suicide to be the solution and the professional the problem. So how does the professional go about reconciling these two positions?
Expert: Reconciling these two positions, life and death, problem and solution requires mindful clinical practice. Remember that the person thinks that life is the problem, death is the solution.
Problem vs Solution
Most people with mental health challenges have a degree of apprehension before reaching out or accepting help. During a serious suicidal crisis, there is a step change in the magnitude of ambivalence the person feels towards an offer of support (Britton et al. 2008). The death orientation of the person in suicidal distress emanates from a belief that suicide is the solution to unbearable psychological pain (Shneidman 1993). In contrast, the professional has a life orientation, believing suicide to be the problem that ends all solutions (Duffy, Ryan 2004).
Host: These are two extremely divergent positions. Attempts to frame suicide as the problem when the person in distress perceives it as potential pain relief, would it not make the distressed individual even more entrenched in their position?
Expert: Exactly and then it will be followed by an unhelpful power struggle. Jobes (2006) articulates how many professionals work from the position that suicide is not an option. One might be clinically and morally opposed to suicide, but the reality is that suicide is a real option for the person who is overwhelmed by life. Professionals taking up the opposite stance is not only invalidating and non-empathic but is blatantly untrue.
Host: So how does one attempt to establish a middle ground?
Expert: Jobes (2006) suggests an explicit discussion about commitment to treatment. In it, patients in suicidal distress are not asked to give up on suicide but to temporarily suspend suicide as an option while they fully engage with treatment, giving it the time and opportunity to have an effect. Candidly explaining that if the treatment does not work, they can always return to suicide as an option, thus making the case with openness and honesty that they have nothing to lose and everything to gain.
Positions, Interests, Needs
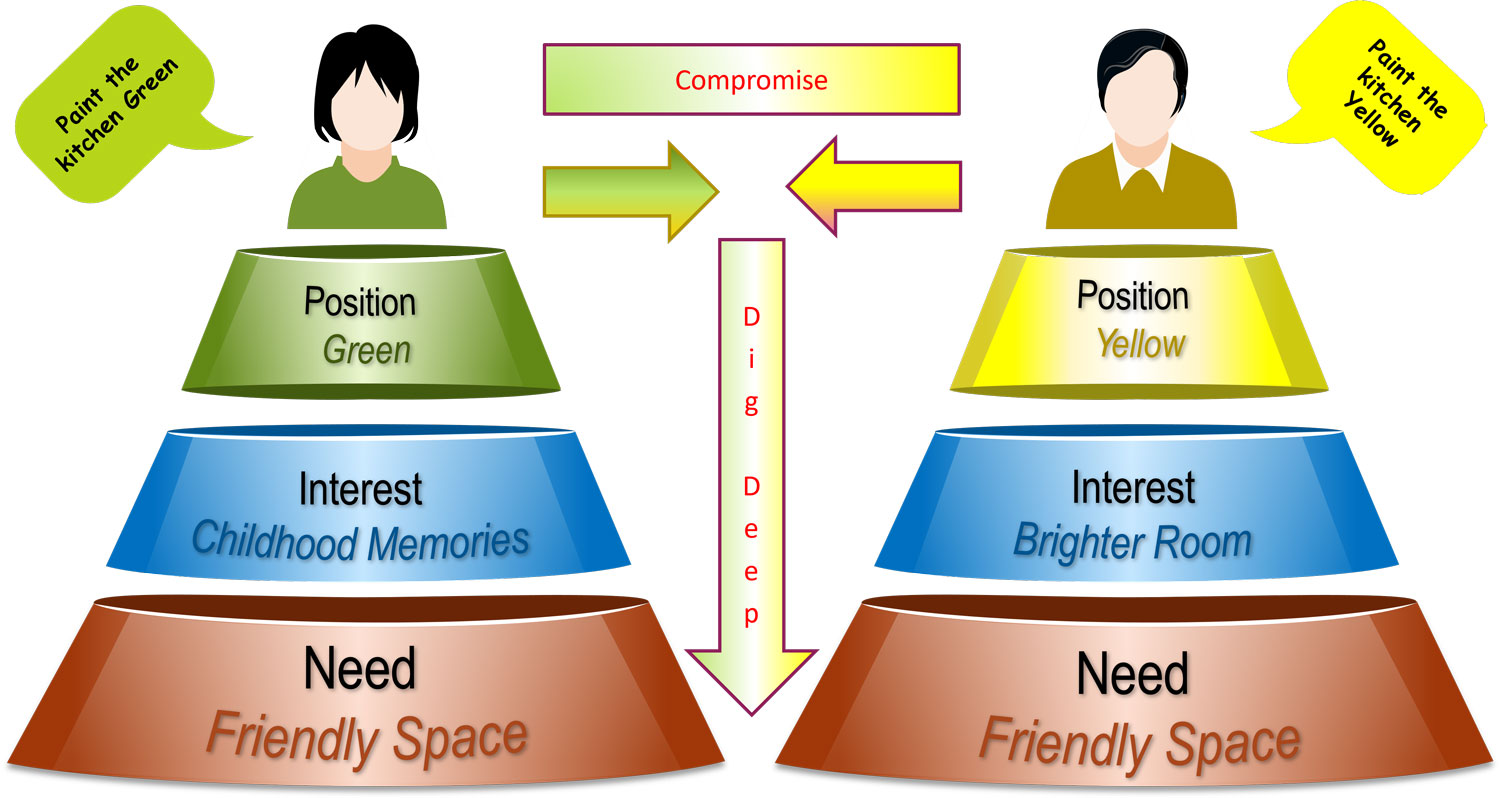
Compromise or Dig Deep
Host: This seems like a fairly nuanced conversation, is there a simple approach or can you break this down for our listeners.
Expert: Consider the case of Mary and Richard, a newly married couple who have bought their first property. Before they move in, they decided to do some decorating. A disagreement ensues over the colour the kitchen should be painted. Mary wants it painted green, but Richard wants it yellow. The disagreement grows into an argument, and neither is in a mood to budge from their position of green and yellow. It is customary in such a situation for one or both to compromise and bring the two positions closer. For example, Mary gets her green kitchen, and Richard can bring with him his star wars collectables which Mary is desperate to get rid of to create more room. From a win-win like this, to two walls green and two yellow, to a lose-lose blue kitchen where no one gets what they wanted, all form different shapes and sizes of compromises.
Host: Sorry I am not following, what has the colour of a kitchen got to do with suicidal distress?
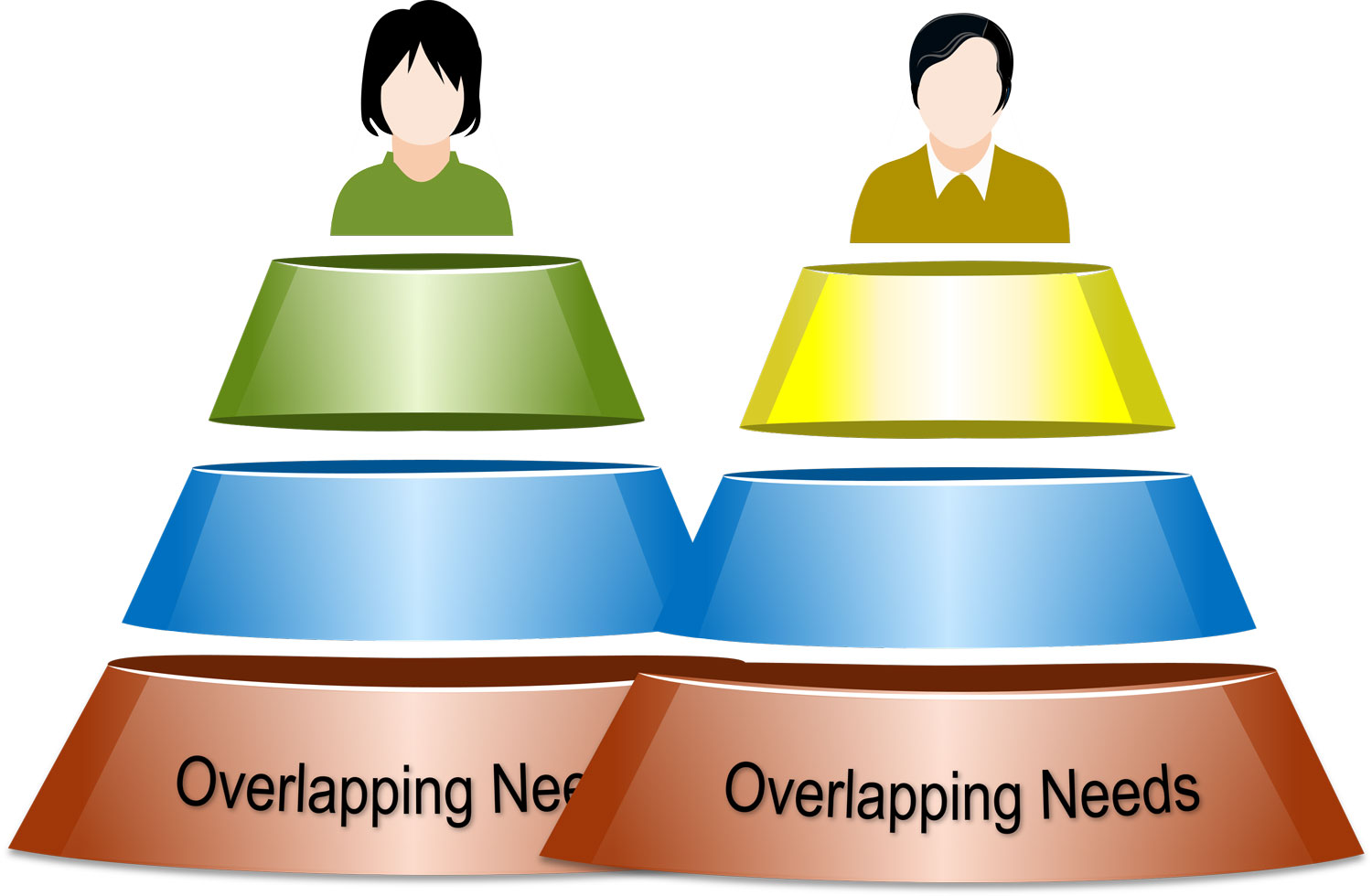
Expert: Stick with me, there is a point to the story. Instead of compromising, Mary and Richard could take an alternative approach to dig deep and understand what lies beneath the entrenched positions of green and yellow. Mary says, “I grew up with a green kitchen, and I have so many happy memories. Painting it green will make it a friendlier space.” Richard replies, “The room is quite dark. Painting it yellow will make it brighter and will make it a much friendlier space.” These interests underlie the positions of green and yellow. In fact, both have a need for a friendlier space. Digging deep often reveals overlapping needs. Understanding each other’s position in terms of interests and needs may help gain an alternative perspective with common ground.
Host: Surely you are not equating a disagreement over the colour of a kitchen to the power struggle that ensues between a professional and person in suicidal distress.
Expert: The example might seem trivial, but one can apply the same logic to more serious issues, lets take it up a notch, e.g. parenting styles, a father and mother may have very different approaches, one may be strict and directive and the other may come across as lenient putting responsibility on the child to do the right thing, but both have the same need, that is to have a happy thriving child or young adult who is living life to their potential. The parents could enter into a power struggle, blaming each other for their teenage son or daughter’s rebellious behaviour or could attempt to understand what lies below each other’s position and approach and whether there is a common ground where they can meet and be a team and work towards a shared horizon.
Host: So in this rather simplified problem of a green or a yellow kitchen, there may be clues as to how we navigate the more complex dissonance between suicide the solution and suicide the problem.
Dissonance to Resonance
Expert: Exactly, to gain an alternative perspective into the mind of a person in suicidal distress, we recommend a similar approach where the professional digs deep to establish the interests and needs that underlie the position of dying. When faced with the ambivalence a person is experiencing towards life, it is strongly recommended to avoid a power struggle. Professionals need to temporarily relinquish their strong desire to pull over the person from their death orientation to one of living. This requires courage as it might go against all that the professional believes in and is trained in.
Host: You are saying curb this urge and dig deep?
Expert: and gain an understanding of how the underlying interest to escape entrapment and the need to be pain-free manifests as suicidality. Construct a pain based narrative and help the person see that their desire to eliminate excruciating pain is a justifiable response, a response they share with all other living beings. This validation will go a long way in establishing the safety partnership. But above all, seek first to understand and then to be understood.
Host: seek first to understand and then to be understood, is this at the heart of relational safety?
Expert: Yes, seeing the world from the person’s view can help the partnership get through some trying times ahead. The conversational skills needed to navigate ambivalence without activating resistance are covered in detail under Motivational Interviewing (MI) strategies in the ASPIRE module, we have a chapter on Acceptance. Open questions, Affirmations, Reflections and Summaries, in short called OARS skills from MI will help the professional connect the position, interest and need for the person in suicidal distress. Explicitly articulating to the person why a pain guided desperate measure seems like a reasonable response is healing in its own right.
Host: But surely, encountering suicidality activates the professional’s desire to jump in and rescue.
Expert: Yes, They want to help a person in pain be pain-free. So the professional begins to explain alternatives to suicide prematurely. The challenge of empathy demands that professionals do not focus on “what they need to say” but “what the other needs to hear”.
Host: So what does the other need to hear?
Expert: What a mind in crisis needs to hear is an empathic acceptance, that their suicidal desire, their thoughts and actions are undertaken in the interest of escaping entrapment and the need to be pain-free. The professional must comprehend this connection first. If they do, not only can they understand the apprehension to the offer of help in terms of life and living (i.e. safety) as it equates to more pain, they can then guide the person to see how in their desire to eliminate the pain they are eliminating life.
Host: So, I am assuming that validating the suicidal distress in this fashion opens up the conversation for potential alternatives that are less drastic.
Expert: Yes, In terms of pain relief, they may be much slower than suicide, but they are effective in either chipping away at the pain or improving one’s tolerance to it. When a professional can explain these connections with openness and honesty, not only do they gain the trust of the individual but also the commitment to work together towards a life orientation that does not involve a power struggle, there in constructing relational safety.
Host: How does this differ from conventional risk management training?
Expert: Knowing that a fellow human being has made a genuine effort to understand their predicament and their desire to be pain-free has a healing touch that no paper-based tick box risk assessment can come close to matching (Mulder et al., 2016). Validating the connection between suicide and pain allows for the connection between pain relief and hope to flourish. The person in distress is then more open to forming an alliance that accepts professional expertise as help rather than a hindrance.
Host: An alliance or partnership, does this mean they will be more willing to bring to play their own lived experience and what works for them.
Expert: Spot on, each person’s recovery is individual to them, and thus the unique context is essential. We believe if such an alliance is to be established, it calls for a sensitive but candid dialogue that is framed in terms of the professional’s curiosity to establish “what matters to you”. This will reveal the source of pain and ways in which it can be addressed. Constructing relational safety calls for a value set that is lived in every action, whether that be listening with fascination or using healing words to capture hope.
Host: In conclusion, it seems the objective is to co-create a pain relief narrative that the person has ownership of. Then, through the subtle art of empathic persuasion, the professional takes the person in distress on a journey of guided discovery while candidly explaining that the professional’s role is to find alternative ways of escaping the entrapment. The professional helps the person connect the dots until they see that they want to be pain-free and the professional wants to help them be pain-free. There is common ground between the two, grounds for a partnership.
Expert: This journey of shared discovery makes it abundantly clear that the pain can be chipped away at or the tolerance to it can be improved. This makes it appropriate to keep suicide in abeyance giving treatment a chance to take effect.
Host: Our goal is to transform mental health care by bringing passion to purpose and progress to practice. If you have found the conversational approach of optimising pain relief useful, please do share it with fellow colleagues and ask them to do the same. Your help is vital in changing the way professionals’ approach suicidal distress and making relational safety a core competency for health care professionals. Thank you.
You may also like
19 | Creep Crash Crawl
18 | AWARE 5 – Experience