01 | Introduction to PROTECT: Novel Solutions to Suicide Risk Management
- Posted by Manaan Kar Ray
- Categories Weekly PROTECT Podcast
- Date January 7, 2022
My Personal Narrative
“Wake up, there is an emergency,” said my father. 2021 marks the passage of 20 years since that 5 AM shove. However, I still remember the sight of the beloved family member who had suicided as if it was yesterday. Although I was a young doctor, I was not unfamiliar with death. But the stone-cold touch of a loved one left an indelible mark on my psyche. There was no emergency; it had been a little while since he had passed away.
Two years earlier, I had made the decision to train as a Psychiatrist. Very few supported my carrier path. He was one of them who stood by me. The afternoon before he suicided, we had spent together. I was about to leave for Britain. It is customary in India to take the blessings of elders when one begins a new life journey. We chatted about life, politics, philosophy. We talked about day to day things. His son had a tremor, and he had taken him to a bank manager to ratify his signature on bank cheques. He told me about money that he was putting away in gift envelopes for his grandchildren for the upcoming Autumn festival. It was a pleasant afternoon with nice memories to cherish. Little did I know that he was sharing final acts with me.
Over the years, I have reflected endlessly on that afternoon. At times, I gently remind myself that I was not looking, and he never had any mental health challenges. If anything, he was the model of resilience and wisdom for the entire community. At other times, I tell myself that I do not have the superpower to read minds or foretell the future. How was I to know that having made a final decision, he was at peace? But every now and then, my defences still fall apart as I grapple with self-doubt. Having said that, his memory continues to inspire me and my work.
My passion and work in suicide prevention perhaps emanate from a place of personal pain and loss. It has been shaped by the grit and determination that I have seen in so many people in suicidal distress; they have taught me my most important life lessons. However, it is the likes of you, mental health professionals, who capture hope when hope is fading that I would like to dedicate this book. Dawn heals the darkest hour, but when dawn is not in sight, you are the candle of hope. To you…
Dr Manaan Kar Ray
SUICIDE - THE SOLUTION
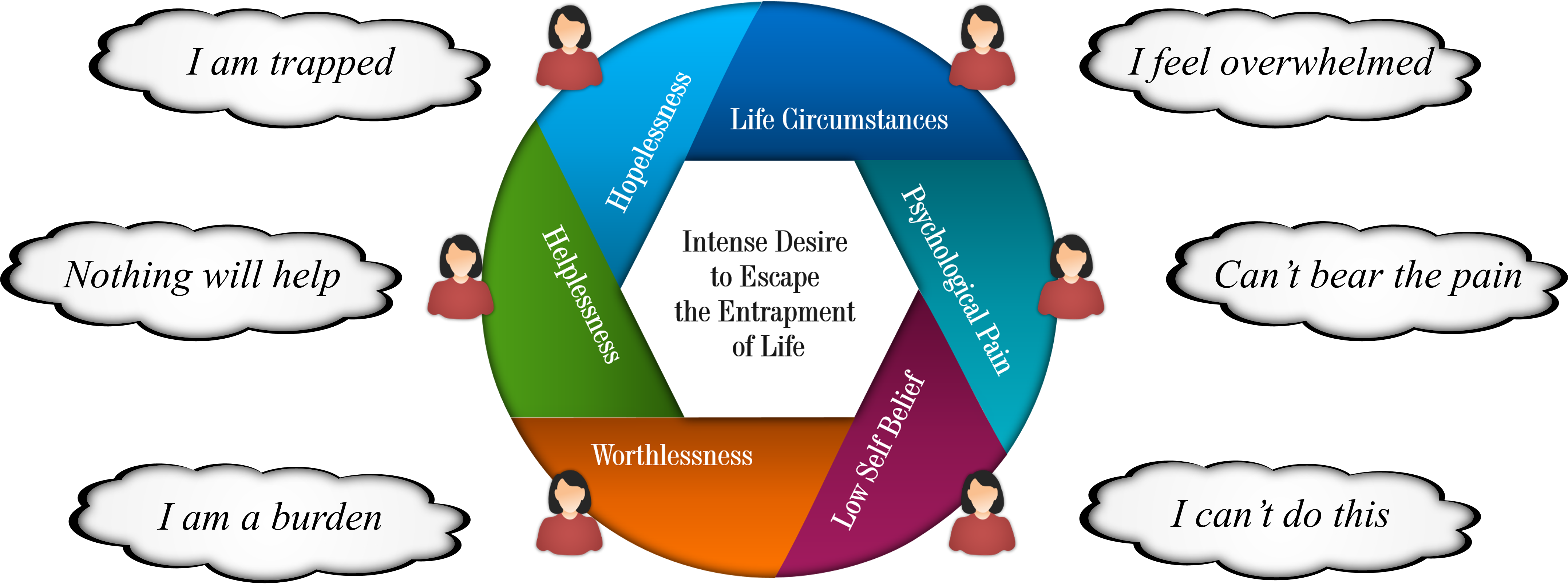
A person with suicidal ideation is often trapped in an overwhelming sense of despair (Beck, 1986). Stemming from entrapment, suicide may become the salient solution to life circumstances (O’connor, 2011) and intense psychological pain (Shneidman, 1993). Suicide is a major public health problem, with over 800,000 people dying annually worldwide, and for each completed suicide, there may have been 20 other attempts (World Health Organization, 2014). To support those in suicidal distress, professionals, families and friends strive to establish new and alternative ways of coping (Jobes, 2006, p. 122; Owens et al., 2011). However, there is a dissonance between the reality of those experiencing a crisis, for whom suicide is the perceived solution, and those that are caring, who view suicide as the problem (Duffy, 2006). Reconciling these positions is difficult as professionals have to understand the person’s pain before they can form a collaborative partnership on the road to recovery (Michel & Jobes, 2011). In a serious suicidal crisis, recovery-oriented practice is often sacrificed on the altar of safety, and care becomes prescriptive. In our previous work in reducing coercion in care in the acute setting (PROMISE), staff and patients highlighted the difficulties in striking this balance. They described the restrictive practice as “it never is very nice… but it is a necessary evil” (Wilson, Rouse, Rae, & Kar Ray, 2017). 86% of study participants highlighted the importance of enhancing relationships through empathic communication as a way of overcoming the challenges posed (Wilson, Rouse, Rae, & Kar Ray, 2018).
This was the most common theme that emerged and formed the foundation of the PROMISE programme, which showed that with the right care, the person has more control (Lombardo et al., 2018). This way of working calls for compassion and a deeply empathic value set amidst professionals who need to be skilled at identifying and supporting people at risk, sometimes in high-pressure environments like inpatient wards and emergency departments (Canner, Giuliano, Selvarajah, Hammond, & Schneider, 2018). Although suicide prevention training to gatekeepers, primary care physicians, emergency department staff and mental health professionals has been rolled out (Albright, Timmons-Mitchell, & McMillan, 2018; Gryglewicz et al., 2019; Hodges, Inch, & Silver, 2001), reducing suicide rates remains a challenge (Arensman, 2017).
Most packages focus on assessment skills, risk screens and risk factor tools (Mortensen, Agerbo, Erikson, Qin, & Westergaard-Nielsen, 2000) but do not address tensions between divergent views of people in distress and professionals involved and how to build empathic partnerships (Downes, Gill, Doyle, Morrissey, & Higgins, 2016) in time and resource-poor environments. Risk assessments may become a tick box exercise and fail to capture the narrative of the person’s distress (Cole-King & Lepping, 2010). Also, most training programmes focus on which information to collect and do not address biases in thinking and attitudes (Owens et al., 2011), which may considerably influence the outcome.
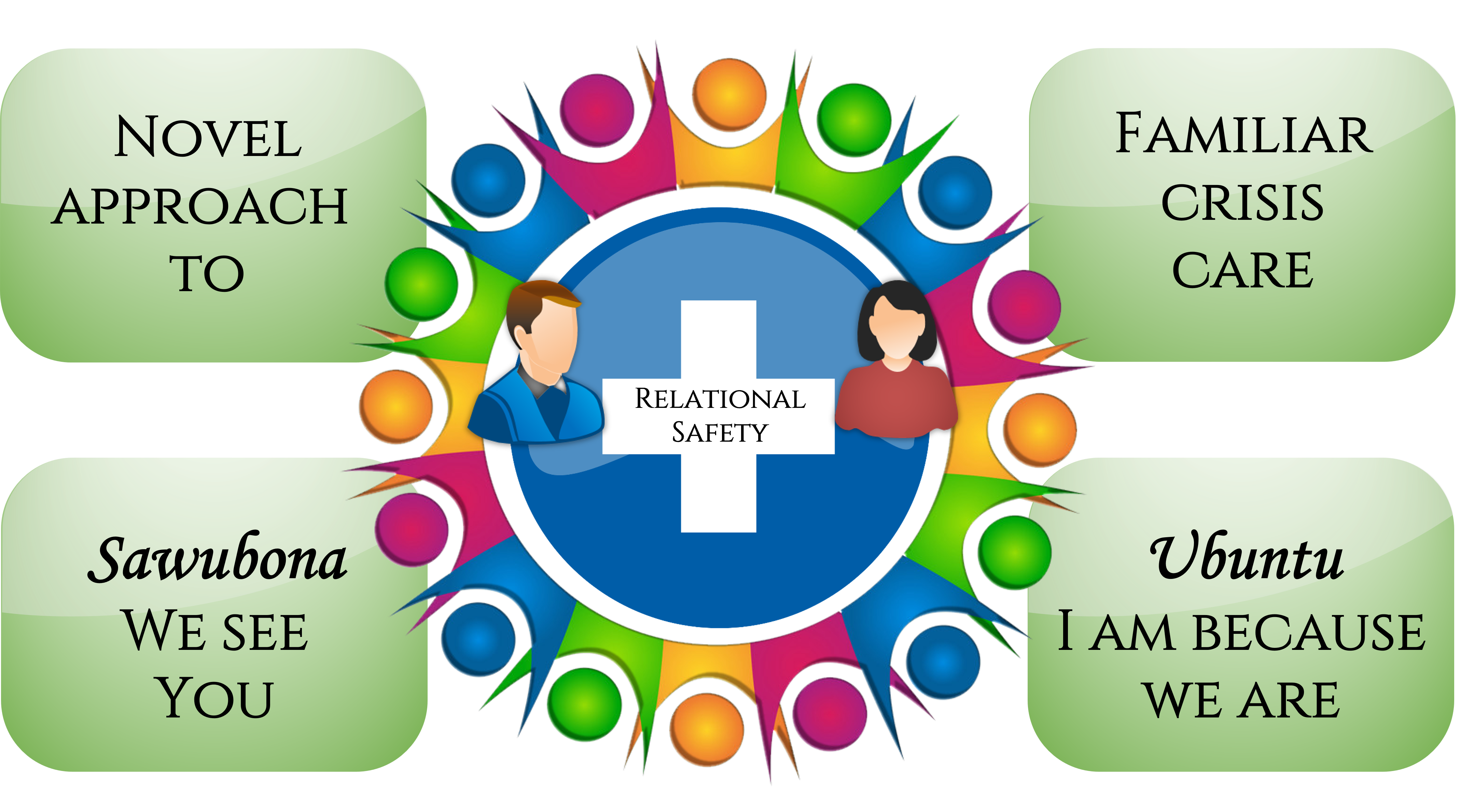
Relational Safety
Based on Relational Safety PROTECT provides a novel approach to familiar crisis care. Relational Safety can be considered a deeply empathic therapeutic alliance that the professional establishes with the person in distress and their natural circle of support. The relationship itself becomes the springboard for recovery. Sawubona (we see you), a Zulu greeting, captures the essence of relational safety. We (me and my ancestors) don’t just see you, we see your ancestors, your world, your hopes, your aspiration, and through the act of seeing, we bring you into being.
Pause for thought: When assessing or supporting people with suicidality, do we see them for who they are and what they stand for in life or do we see a risk that needs fixing?
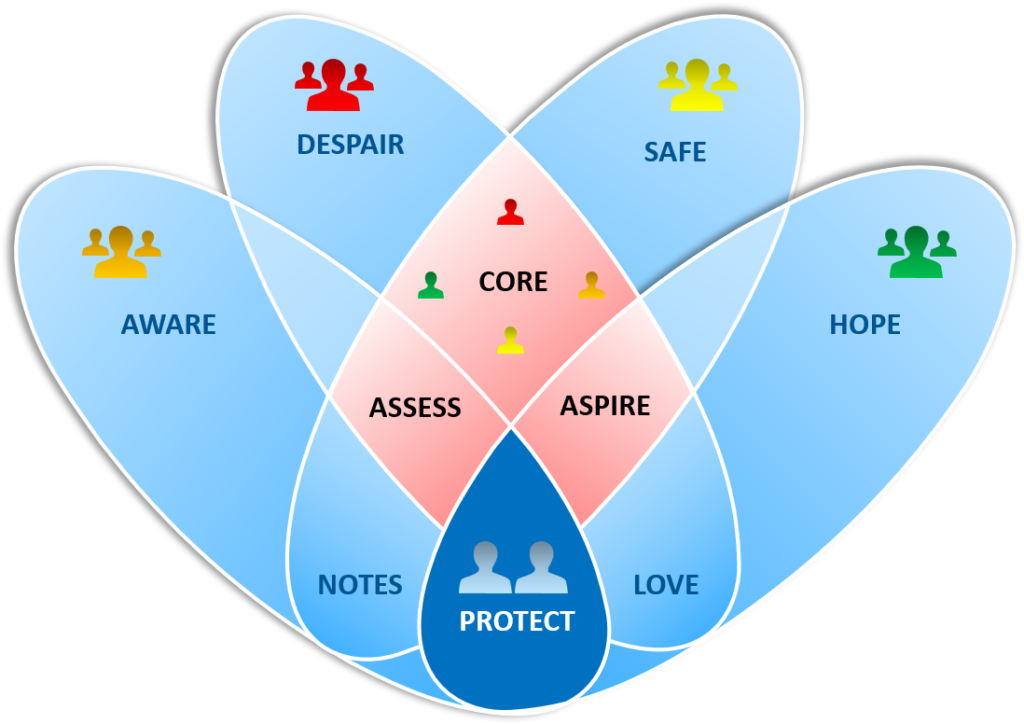
CORE
Protect the CORE, progress all else. The CORE module lays the foundation on which PROTECT is built. It establishes the values and principles of Relational Safety, supporting professionals to strike the delicate balance between risk and recovery. The practice of empathy in action is brought to life through a range of theoretical constructs and conversation aids.
ASSESS
Knowing oneself is a prerequisite to gaining a thorough understanding of the psychological pain of the person in suicidal distress. ASSESS promotes self-awareness regarding clinical decision making, along with knowledge of the assessment sequence, suicide phenomenology, strategies for interactions, all the way to formulation and documentation
ASPIRE
The care module in PROTECT is a framework to co-create a safe and empowering recovery journey. Acceptance of the person’s ambivalence towards living enables a sequence of actions, from safety planning in the midst of a crisis to delivering person-centred care, building resilience for the future. ASPIRE brings to life assets focused, recovery-oriented way of working.
PATIENT EXPERIENCE SCORES FROM PROMISE
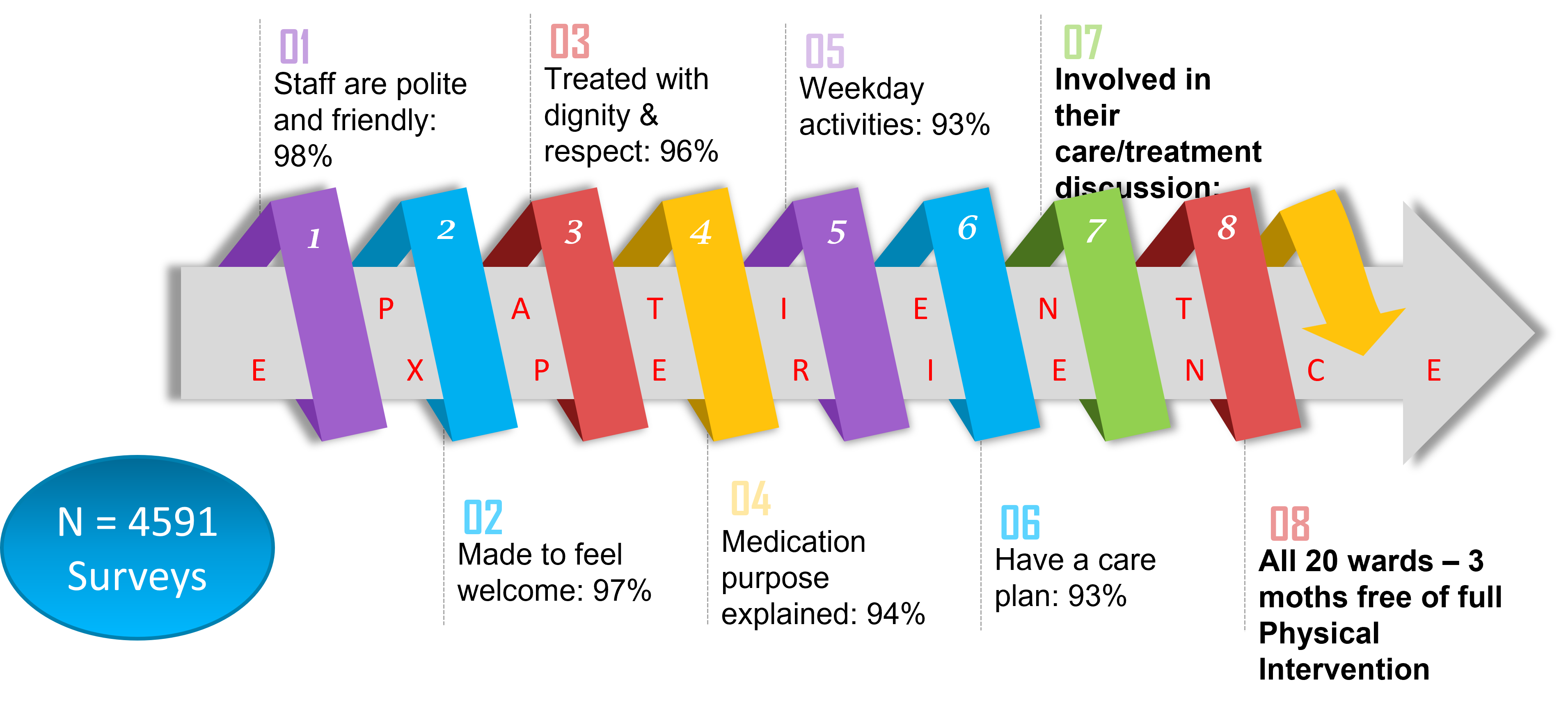
PROTECT (PROactive deTECTion) builds on a model of relational safety and hope vending developed in two successful initiatives (333 and PROMISE) in Cambridgeshire, United Kingdom. The success of 333 (Kar Ray et al., 2019) and PROMISE (Lombardo et al. 2018) hinged on staff establishing a deeply empathic therapeutic alliance and bringing to life the construct of relational safety. Within its scaffold, professionals, the person in distress and their natural circle of support shared a mutual respect for each other and worked towards shared goals, navigating the care vs control dilemma. PROTECT aims to capture the relational way of working embedded in 333 and PROMISE. The four frameworks operationalise this seemingly abstract concept into day to day clinical practice. Without risk, there is no recovery and managing these inherent tensions in decision making between managing risk and supporting recovery is central to the model.
PROMISE
Eliminate Coercion in Care
The national award-winning PROMISE initiative was a values (care, courage and coproduce) based approach to decrease the incidence of physical interventions by enhancing the patient experience. The scores above are a testament to what can be achieved when staff and patients work together towards common goals.
333
Innovative Acute Care
333 is a highly acclaimed, dynamic inpatient and community crisis care system, running in Cambridgeshire, UK, since 2011. It outperforms national averages for safety and clinical efficiency measures, pushing quality up while bringing costs down.
You may also like
19 | Creep Crash Crawl
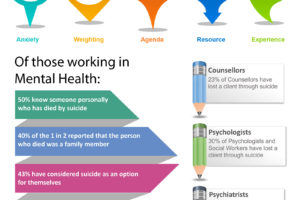
18 | AWARE 5 – Experience